Frequently Asked Questions On Remote Patient Monitoring For Patients & Providers

New to Remote Patient Monitoring (RPM)? Want to improve your knowledge on RPM? Have certain queries about how remote patient monitoring works? If you are curious about RPM and want to understand its dynamics and workflow, here’s some common questions we have drafted to help you go through the ins and outs of remote monitoring and enhance your RPM program outcomes and effectiveness.
- What is Remote Patient Monitoring (RPM)?
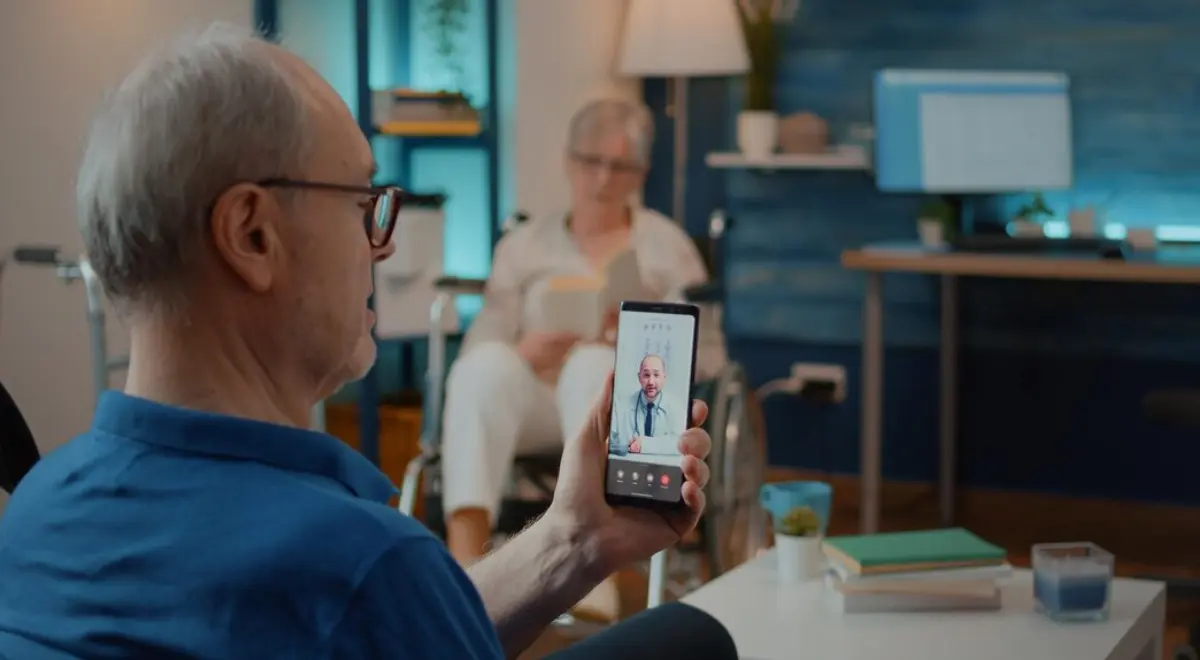
Remote Patient Monitoring (RPM) is a healthcare tool that enables clinicians to monitor patients’ health outside of traditional healthcare venues like hospitals or clinics. It entails using digital technology to collect medical and other health information from patients and securely send it to healthcare practitioners.
- How does remote patient monitoring work?
Remote patient monitoring involves the use of medical devices and sensors to collect health data, including blood pressure, heart rate, and blood glucose levels. Patients can use these devices on their own and record their vitals. The health data is securely transferred to healthcare practitioners who examines it and make required interventions.
- What are the benefits of an RPM program?
- Increased convenience both for patients and providers
- Early detection of health issues
- Improved patient engagement
- Enhanced communication with and amongst healthcare providers
- Reduced hospitalizations and readmissions
- Reduced overall healthcare costs for both patients and providers.
- What chronic conditions are monitored using remote patient monitoring?
Remote Patient Monitoring is ideal for monitoring various chronic conditions, including:
- Hypertension (high blood pressure)
- Diabetes
- Heart failure (CHF)
- Chronic obstructive pulmonary disease (COPD)
- Asthma
- Chronic kidney disease (CKD)
- And other chronic conditions
- What are common remote patient monitoring devices?
There are many RPM devices available and their use varies on the patient’s condition and monitoring requirements. Some common health monitoring devices include:
- Blood pressure monitors
- Blood glucose meters
- Pulse oximeters
- Weight scales
- Electrocardiogram (ECG) monitors
- Peak flow meters (for monitoring lung function)
- Thermometers
- Who can provide and bill for RPM services?
Physicians and other qualified healthcare professionals (QHCPs) can provide and bill for RPM. Clinical staff can monitor patients under the general supervision of a physician or qualified healthcare professional.
- What are steps involved in setting up a successful RPM program?
Each RPM program is unique and so are the steps involved in setting up a successful RPM program. Some general steps providers need to follow include:
- Consult with private payers, Medicare, and Medicaid to determine coverage
- Consider who you will accept as RPM patients
- Identify the chronic conditions you will manage
- Choose the devices you’ll use to provide RPM services
- Set up an intake method to start the patient care process, instruct them on how to use an RPM device, and address any queries that arise
- Establish RPM policies and processes.
- Train your staff on monitoring and recognizing symptoms that need intervention.
- How does remote patient monitoring differ from telehealth?
RPM is considered a subcategory of telehealth. The term ‘telehealth’ can be used to refer to RPM, but it can also refer to a wide range of other remote healthcare services. RPM is the use of technology to facilitate communication between providers and patients outside of the clinical settings.
- How to ensure an RPM program is HIPAA compliant?
Before investing in an RPM program, thoroughly investigate the RPM vendors and their devices. Vendors need to make sure the patient data is encrypted while in transit from patient to provider and even when the device storing the data is not in use.
- What should I do if I notice unusual changes in my health data?
You should notify your healthcare professional right away if you observe any unusual changes in your health data, such as variations in your vital signs. They will make the necessary intervention by making changes to your treatment plan or setting up a face-to-face session for additional assessment.
- How can I sign up for a remote patient monitoring program?
Consult your healthcare practitioner about becoming a member of a remote patient monitoring program. After determining whether RPM is appropriate for your medical needs, they will send you details on how to take part in the program.
- What chronic cases are monitored using remote patient monitoring?
- Cardiology
- Pulmonology
- Endocrinology
- Gastroenterology
- Bariatrics
- Diabetes
- Neurology
- Obesity
- Oncology
- Retina
- Hypertension
- Congestive Heart Failure (CHF)
- Chronic obstructive pulmonary disease (COPD)
- Is it possible to bill RPM along with chronic care management (CCM)?
Providers can bill both the CCM CPT code 99490 and the RPM CPT code 99457 together. A provider must offer at least 40 minutes of services—20 minutes of RPM and 20 minutes of CCM—in order to bill 99457 and 99490 combined, avoiding double counting.
- What CPT codes are covered by the RPM?
- 99453 (One time code to set up the patient on RPM)
- 99454 (Devices supply with daily recordings or programmed alerts transmission)
- 99457 (Remote physiologic monitoring treatment management services)
- 99458 (Add-on code for remote physiologic monitoring treatment management)
- 99091 (bill for “complex” RPM management)
- What are the documentation requirements for RPM?
To document RPM, the documentation requirements include:
- patient consent
- practitioner order for device deployment
- conditions for which the patient is being monitored
- device identification
- date of delivery of the device to the patient
- date on which training is provided to the patient
- Is it possible for multiple providers to provide remote patient monitoring services to same patient at the same time?
No. There has been a lot of misunderstanding and buzz about this topic. Assisting and billing patients who are already getting remote patient monitoring services from another provider will probably result in the denial of claim. Issues with compliance may arise if billing for RPM is attempted repeatedly in this manner.
- Can I bill for RPM and RTM together?
No, it’s not possible.
- Are RPM codes subject to patient co-pays?
Yes, patients pay the applicable coinsurance based on the services received.
- Are RPM codes only for people with chronic conditions?
No, the codes are not limited to particular conditions/ chronic diseases or medical specialities.
- Can RPM be used with both new and established patients?
According to CMS’ 2021 Final Rule, RPM services are only available to “established patients.” At the start of COVID-19, CMS eliminated the “established patient” criterion, stating that practitioners might give RPM services without first performing a new patient E/M. Billing Medicare for CPT 99452, 99454, 99457, and 99458 requires an established patient practitioner relationship.
So, there are some of the most frequently asked questions about remote patient monitoring we have compiled. If you still didn’t find the answer to your query, feel free to contact us for a consultation.
Interested in our remote patient monitoring software? Book a HealthArc demo to find out how it works.
Most recent blogs
Categories
- Behavioral Health Integration
- Cellular Remote Patient Monitoring
- Chronic Care Management
- Chronic Care Management Billing
- Chronic Care Management CPT Codes
- Chronic Care Management Program
- Chronic Care Management Software
- Digital Health Platform
- Principal Care Management
- Principal Care Management CPT Codes
- Remote Monitoring Devices
- Remote Patient Care
- Remote Patient Monitoring
- Remote Patient Monitoring Billing
- Remote Patient Monitoring CPT Codes
- Remote Patient Monitoring Devices
- Remote Patient Software
- Remote Therapeutic Monitoring
- Remote Therapeutic Monitoring Billing
- Remote Therapeutic Monitoring CPT Codes
- Telemedicine & RPM
- Transitional Care Management
- Transitional Care Management Billing
- Transitional Care Management CPT Codes
Related Posts
- July 23, 2024 | Read Time: 8 mins
HealthArc Vs. Prevounce: Which One To Choose?
- July 4, 2024 | Read Time: 6 mins
Remote Patient Monitoring for Alzheimer’s
- June 21, 2024 | Read Time: 5 mins