How to Choose the Best Weight Scale for Remote Patient Monitoring

Imagine this: You’re reviewing the remote monitoring data of a patient with a chronic condition, and something doesn’t quite add up. The readings are inconsistent, leading to a moment of doubt about the treatment plan you’ve so carefully crafted.
This scenario is all too familiar in the world of Remote Patient Monitoring (RPM). The culprit? Often, it’s the choice of RPM scale.
As a healthcare professional who’s navigated the complexities of patient care for years, you know that the right tools, especially remote health monitoring devices, are crucial for accurate monitoring.
But with the plethora of RPM scales available, each promising the best results, making the right choice can be daunting. It’s not just about numbers and data; it’s about the lives and well-being of your patients.
In this guide, we’ll walk through the maze of RPM scale selection together. We’ll explore what makes a scale reliable, how to match it with patient needs, and why the right choice can make all the difference in your patient remote monitoring strategy.
Let’s embark on this journey to ensure that your remote patient monitoring is as precise and effective as your in-person care.
Table of Contents
ToggleWhat is a Remote Patient Monitoring Scale?
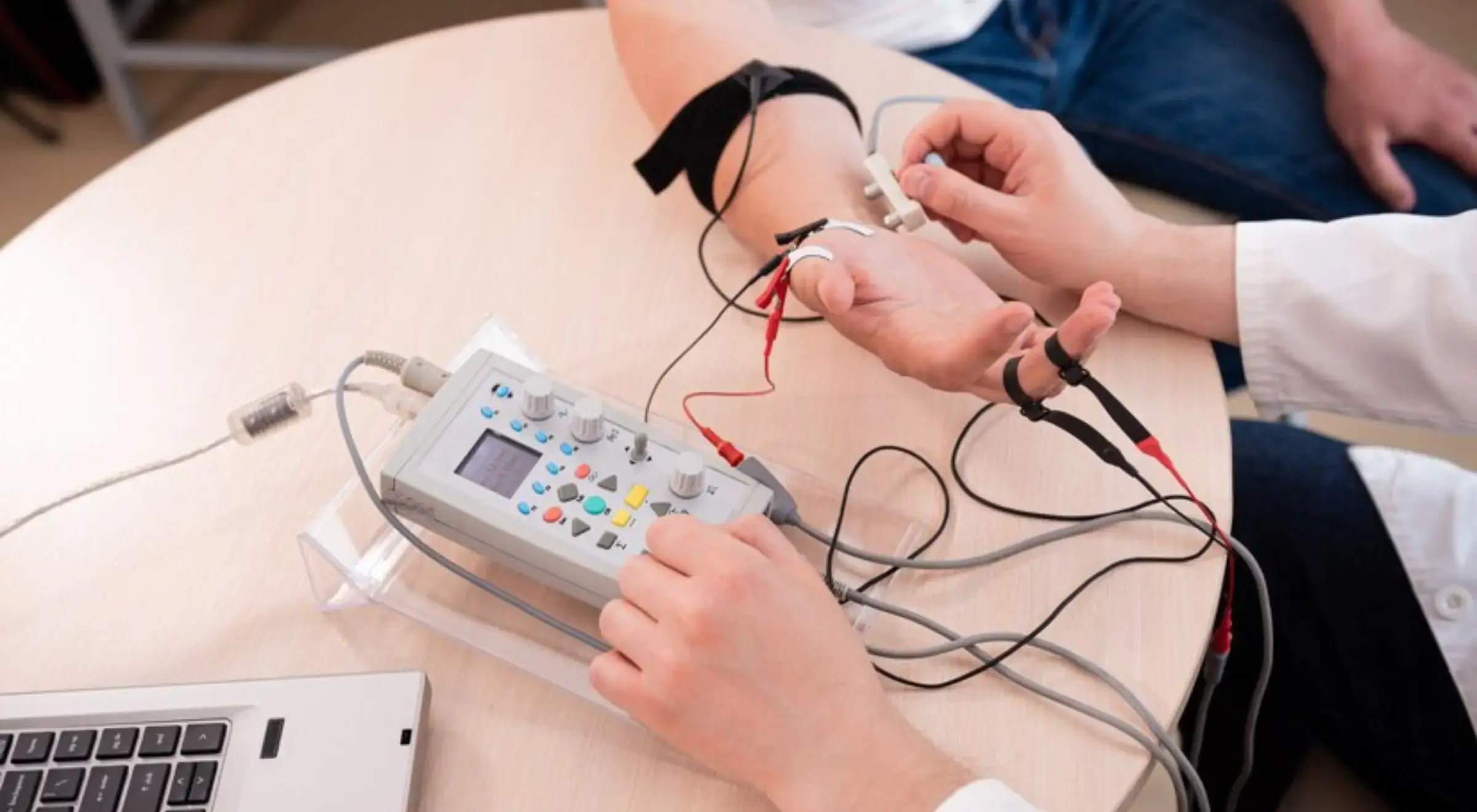
Remote Patient Monitoring (RPM) is a method of healthcare delivery that collects patient data outside of traditional healthcare facilities by utilizing cutting-edge information technology.
It typically involves the use of various medical remote patient monitoring devices, including scales, to monitor health-related data such as weight, blood pressure, heart rate, blood sugar levels, and more.
This data is then transferred securely to healthcare providers for assessment, allowing for continuous monitoring of patients, particularly those with chronic conditions.
A Remote Patient Monitoring (RPM) scale is among the most technologically advanced medical monitoring devices designed to measure and record a patient’s weight and other health-related metrics.
Unlike traditional scales, an RPM scale is equipped with smart features that allow it to transmit this data remotely to healthcare providers.
What Makes RPM Scales Different From Traditional Weight Scales?
Remote Health Monitoring scales represent a significant leap from traditional weighing scales, both in functionality and in their role in patient care.
To understand their unique value, let’s explore what sets RPM scales apart and why they are indispensable in modern healthcare settings:
Integration with Predictive Analytics and AI
Unlike standard scales, RPM scales often integrate with predictive analytics and AI algorithms.
This integration allows for advanced health risk assessments, such as predicting exacerbations in chronic conditions like heart failure through detailed analysis of weight and other biometric fluctuations.
Advanced Sensor Technology for Enhanced Accuracy
RPM scales utilize sophisticated sensor technology that surpasses the basic weight measurements of traditional scales.
These sensors can detect minute changes in biometric data, offering critical insights into a patient’s health trends and enabling early intervention in disease management.
Real-Time Data Synthesis and Interpretation
A key differentiator of RPM scales is their ability to synthesize and interpret data in real time.
This feature facilitates immediate adjustments in patient care plans, which is crucial for conditions requiring close monitoring, such as kidney disease or fluid retention issues.
Seamless EHR System Integration
RPM scales are designed for interoperability with Electronic Health Records (EHR), ensuring that patient data contributes to a comprehensive health record.
This contrasts with traditional scales, where data often remains isolated and underutilized.
Customization for Specific Patient Needs
RPM scales offer customization to address various patient-specific conditions, a feature rarely found in standard scales.
This includes design adaptations for patients with mobility issues, ensuring that the scales are not just measurement tools but integral components of personalized care plans.
Enhanced Data Security and Compliance
In the realm of RPM, data security and compliance with regulations like HIPAA are paramount.
RPM scales are equipped with robust security protocols, ensuring the protection of sensitive patient data, a critical aspect often overlooked in conventional scales.
10 Factors To Consider For Selecting The Best RPM Scale
For seasoned healthcare professionals well-versed in RPM technology, selecting the right scale involves delving into sophisticated criteria that go beyond basic functionalities. Here are the ten key advanced considerations:
1. High-Resolution Data Analysis
Choose scales that offer high-resolution data capture, enabling detailed trend analysis and anomaly detection. This is crucial for managing complex chronic conditions where minute changes can have significant implications.
2. Interoperability with Advanced EHR Systems
Ensure the scale’s compatibility extends to advanced EHR systems and remote patient monitoring software, facilitating deeper data integration. This includes the ability to synchronize with predictive analytics tools and support advanced data mining techniques.
3. Customizable Alert Parameters
Opt for scales that allow customization of alert thresholds and parameters. This enables personalized monitoring, which is especially important in managing patients with multiple or complex health conditions.
4. Integration with Telehealth Platforms
In an era where telehealth is becoming increasingly prevalent, select scales that integrate seamlessly with telehealth platforms and remote patient monitoring systems, enhancing remote consultations with real-time data.
5. Advanced Patient Engagement Features
Consider scales that include features to enhance patient engagement, such as interactive interfaces or integration with patient health apps. This can improve compliance and patient involvement in their health management.
6. Scalability for Practice Growth
Evaluate the scale’s scalability and how it fits into your practice’s growth plan. The chosen technology should be adaptable to expanding patient loads and evolving healthcare services.
7. Sophisticated Data Encryption and Security Protocols
Given the sensitivity of health data, prioritize scales with the most advanced encryption and security protocols. This is critical in safeguarding patient information and maintaining trust.
8. Evidence-Based Clinical Validation
Look for scales that are backed by evidence-based clinical validation, ensuring that the technology is not just innovative but also clinically effective and reliable.
9. Long-Term Vendor Reliability and Support
Assess the long-term reliability and support provided by the vendor, including software updates, technical support, and training for new features or integrations.
10. Cost-Effectiveness in the Long Run
Finally, consider the long-term cost-effectiveness of the scale, including maintenance, software updates, and the potential need for future upgrades.
10 Ways to Utilize Remote Patient Monitoring Scales In Your Practice?
1. Conduct Advanced RPM Scale Workshops
Organize or attend advanced workshops focused on RPM scale technology. These should cover in-depth aspects like interpreting complex data, integrating scales with other remote monitoring devices, including remote blood pressure monitoring systems, and troubleshooting common issues.
2. Develop a Protocol for RPM Data Integration
Create a detailed protocol for how RPM data will be integrated into patient care plans. This should include guidelines on data interpretation, response times for abnormal readings, and documentation practices.
3. Set Up a Multidisciplinary RPM Team
Form a dedicated team comprising members from different specialties (e.g., nursing, IT, administration) to manage and optimize the use of RPM scales. Regular meetings can facilitate knowledge sharing and address any challenges.
4. Implement Customized Patient Onboarding
Develop a comprehensive onboarding process for patients new to RPM scales. This should include personalized training on using the device, understanding the data, and knowing when to alert healthcare providers.
5. Regularly Review and Update RPM Practices
Schedule periodic reviews of your RPM practices. Use these sessions to assess the effectiveness of the scales, update protocols based on new research or technology, and incorporate feedback from staff and patients.
6. Leverage RPM Data for Research and Quality Improvement
Use anonymized RPM data for internal research to identify trends, improve patient care protocols, and contribute to broader medical research in your field of expertise.
7. Enhance Patient Engagement Strategies
Integrate RPM scales into your patient engagement strategies. Use the data to have informed discussions with patients about their health progress and involve them actively in their care plans.
8. Stay Informed About Regulatory Changes
Keep up-to-date with any regulatory changes related to RPM, ensuring that your practice remains compliant with data privacy laws and other healthcare regulations.
9. Evaluate the Financial Impact of RPM Scales
Regularly assess the financial impact of RPM scales on your practice, including reimbursement patterns, cost savings from reduced hospitalizations, and potential for practice growth.
10. Foster a Culture of Continuous Learning
Encourage a culture of constant learning and adaptation within your practice. Stay informed on the latest technologies to further enhance the use of RPM scales.
Ready to Weigh Up Your RPM Practice?
In wrapping up our exploration of RPM scales, remember that the right choice can elevate patient care in your experienced hands.
Speaking of elevating patient care, HealthArc is at the forefront of this mission with its range of cellular-connected devices.
HealthArc offers a variety of devices including a Blood Pressure Monitor, Glucometer, Weight Scale, Thermometer, and Pulse Oximeter, all designed to seamlessly integrate into your RPM practice.
These devices are not only modern and easy to use but also come with the convenience of cellular connectivity, meaning no hassle with apps, pairing, or data syncing.
With HealthArc, you can get started in minutes, not days, ensuring that your patients receive the best care promptly.
For more insights and strategies on enhancing your RPM practice, don’t miss our comprehensive guide on Remote Patient Monitoring Success.
Most recent blogs
Categories
- Behavioral Health Integration
- Cellular Remote Patient Monitoring
- Chronic Care Management
- Chronic Care Management Billing
- Chronic Care Management CPT Codes
- Chronic Care Management Program
- Chronic Care Management Software
- Digital Health Platform
- Principal Care Management
- Principal Care Management CPT Codes
- Remote Monitoring Devices
- Remote Patient Care
- Remote Patient Monitoring
- Remote Patient Monitoring Billing
- Remote Patient Monitoring CPT Codes
- Remote Patient Monitoring Devices
- Remote Patient Software
- Remote Therapeutic Monitoring
- Remote Therapeutic Monitoring Billing
- Remote Therapeutic Monitoring CPT Codes
- Telemedicine & RPM
- Transitional Care Management
- Transitional Care Management Billing
- Transitional Care Management CPT Codes
Related Posts
- December 21, 2023 | Read Time: 6 mins
Guide to Remote Patient Monitoring Success
- October 7, 2022 | Read Time: 4 mins
Five Remote Patient Monitoring Devices
- June 9, 2022 | Read Time: 6 mins