What is Chronic Care Management: A Complete Guide 2025

Every patient counts when you operate a small healthcare facility. However, patients managing multiple chronic illnesses pose a serious challenge to the personalized care delivery model. From coordinating appointments to ensuring timely interventions, all without putting a strain on the staff can be overwhelming for small practices.
Nearly 60% of U.S. adults suffer from a chronic condition, while over 40% juggle with two or more. Their treatment accounts for 90% of the nation’s annual healthcare expenditures. Yet, many small practices struggle to get the resources and infrastructure required to engage these high-need patients efficiently.
Chronic Care Management (CCM) is a benchmark solution that offers continuous support to such patients while initiating a new revenue stream for providers. It offers a scalable way for solo practitioners and small clinics to enhance their care quality. In today’s blog, we’ll walk you through Chronic Care Management. We’ll discuss who it serves and how, and the ways your clinic can seamlessly implement it.
Chronic care management (CCM) is managing a patient’s multiple (2 or more) chronic conditions expected to last at least 12 months, or until their death. Chronic conditions place the patient at significant risk of death, acute exacerbation or decompensation, or functional decline. CCM is a critical primary care service that contributes to better patient health and care.
Table of Contents
ToggleTreatment Beyond Clinic Walls: What Is Chronic Care Management (CCM)?
For patients with multiple chronic illnesses, juggling doctor visits, medications, and lifestyle changes is formidable. To address this issue, the Centers for Medicare & Medicaid Services (CMS) introduced Chronic Care Management. It offers a consistent, virtual care coordination that is effective and round-the-clock. CCM aims to bring about better outcomes and improved patient satisfaction.
CCM services don’t include in-person office visits, offering patients flexibility and comfort during treatment and disease management. By focusing on care coordination, medication management, and extended access to care, CCM ensures that patients don’t have to wait for the next clinic appointment to feel better.
Who Qualifies for Chronic Care Management Services?
The CMS mapped out CCM care for patients dealing with complex and multiple health challenges. Here’s what the core criteria to be eligible for CCM look like-
- Medicare Beneficiaries- CCM is a program supported by Medicare, and thus, only individuals enrolled in Medicare Part B are eligible.
- Two or More Chronic Conditions- Beneficiaries must have two or more chronic conditions which each expected to last at least 12 months or the end of a lifetime, whichever is sooner. Qualifying chronic issues include diabetes, hypertension, asthma, depression, heart failure, etc.
- Conditions Posing Significant Health Risk- Along with the presence of the chronic conditions, they must place the patient at a significant risk of death, acute exacerbation or decompensation, or functional decline to be considered eligible for CCM.
- Informed Consent- Providers must clearly inform the patients about the nature of the CCM services. This includes the services, applicable cost-sharing responsibilities, and data and privacy concerns. This needs to be documented in the medical record.
Note: Providers must initiate Chronic Care Management services during a
- Comprehensive Annual Wellness Visit (AWV), OR
- Routine Evaluation and Management visit (E/M), OR
- Face-to-Face Visit
This ensures that the patient receives foundational care and education before moving ahead with ongoing chronic care support.
The eligibility criteria ensure that CCM services are offered to patients who truly require long-term coordinated care.
Is CCM Right For Your Patients?
The Centers for Medicare & Medicaid Services does not have a finalized list of chronic conditions eligible for CCM. Deciding eligibility depends on the providers based on the type of conditions. However, the ailment must be expected to persist for anywhere between 12 months and a lifetime. Common chronic conditions which are covered under CCM eligibility include-
- Diabetes
- Hypertension
- Congestive Heart Failure
- Asthma
- Arthritis
- Chronic Obstructive Pulmonary Disease
- Hyperlipidemia
- Depression and relevant mental health issues
The broad definition allows providers to tailor care plans to treat one or more chronic illnesses virtually. This helps improve patient health and prevent the ill effects of conditions that affect their daily functioning and overall well-being.
As per the Centers for Disease Control and Prevention, 6 out of 10 U.S. adults have at least one chronic illness, while 4 out of 10 have two or more. These startling figures indicate the need for Chronic Care Management to support eligible beneficiaries in tackling chronic conditions.
Why Is CCM Important for Patients with Long-Term Conditions?
Patients, especially senior citizens, often struggle to manage their health and adhere to their treatment plans. Visiting clinics regularly isn’t feasible, and they tend to miss medications, misunderstand care instructions, or defer seeking help until conditions worsen. Consequently, providers experience more emergency room visits and hospital admissions, and patients, unknowingly or knowingly, lead a deteriorating quality of life.
By offering proactive, consistent, and coordinated support to such patients, Chronic Care Management bridges these gaps in healthcare. It virtually provides patients with a point of contact where they can answer questions, monitor symptoms, and adjust medications or treatment plans as required. This empowers them to stay on track with their care plans and lead a healthy life.
Key benefits of CCM include-
- Improved adherence to medication and treatment plans through regular follow-ups.
- Better disease management and improved patient outcomes through early detection of complications.
- Reduced emergency hospital readmissions by following preventive measures.
- Increased patient satisfaction through constant virtual engagement and round-the-clock support.
- Enhanced care continuity across all healthcare stakeholders and providers.
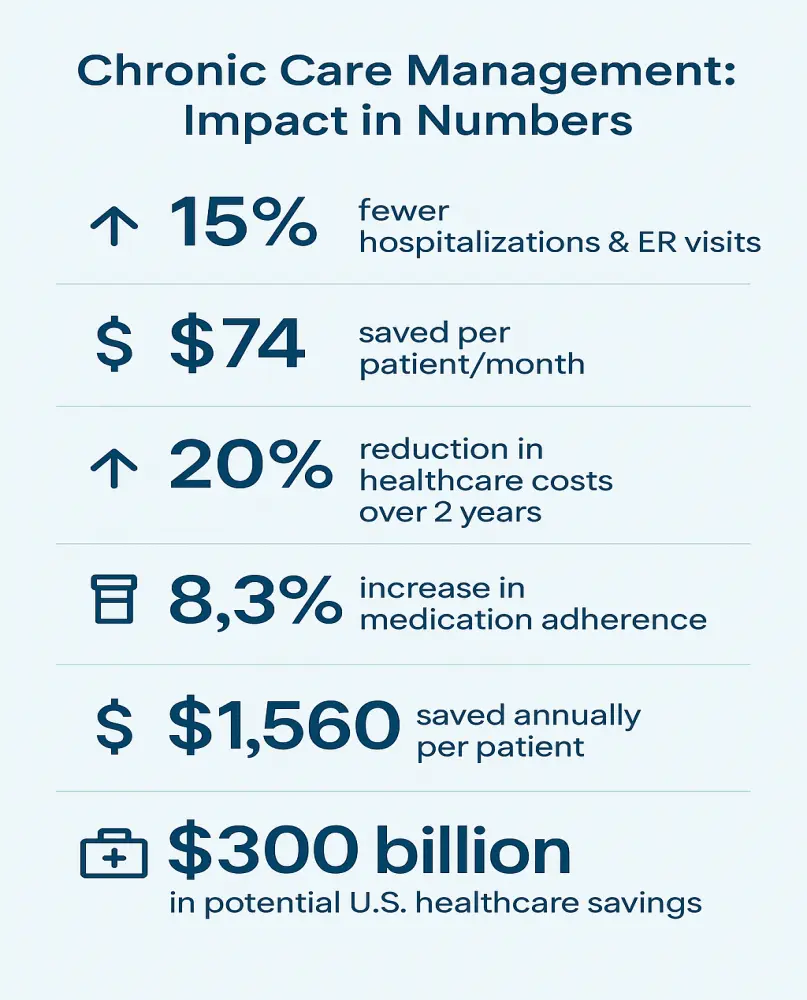
Case Study- CCM helps reduce hospitalization by 15%
With the goal of dealing with emergency room visits and hospital readmissions in the case of patients with chronic illnesses, the Centers for Medicare & Medicaid Services introduced Chronic Care Management in 2015. It focused on offering non-face-to-face care coordination to patients with one or multiple chronic ailments. Providers embedded it into their care services, and enrolled patients started receiving personalized care plans with 24/7 access to healthcare support and regular virtual monitoring.
In a 2021 study conducted by the American Journal of Managed Care, it was revealed that patients participating in CCM programs witnessed a 15% reduction in hospitalizations compared to non-participants. Improved clinical outcomes accompanied this in terms of delaying serious health events and cost savings for the patients.
The CMS also reported annual net savings of $74 per patient after adhering to CCM practices. Moreover, CCM helped reduce healthcare costs by 20% over two years, according to a study published in the Journal of Medical Economics.
This Case Study underscores the role of CCM in managing chronic illnesses, offering health and financial benefits to patients, providers, and the U.S. healthcare system.
Behind the Scenes: How Does Chronic Care Management Work in Practice?
Chronic Care Management is a team-based model focused on offering patient-centric services beyond the clinic walls. Here’s how CCM works once a patient is enrolled-
- Care Plan Development: Physicians and providers develop a comprehensive care plan based on patients’ health conditions, treatment goals, and medical history. The plan includes prescribed medications and self-management strategies to ensure compliance with the treatment plan from both ends. Patients also receive access to community services or specialists for a result-oriented ongoing healthcare program.
- Electronic Health Record Integration: Documenting patient-provider communication and the comprehensive care plan is essential. The providers create an Electronic Health Record (EHR) in the system to ensure accurate information sharing among all stakeholders and for future reference.
- 24/7 Access to Care Coordination: Enrolling in a CCM plan ensures 24/7 access to urgent care services and clinical support for patients. They can reach out to experts in times of need and query, and providers are obliged to provide timely assistance whenever their health status changes.
- Continuous Virtual Care: Patients enrolled in the CCM program receive a minimum of 20 minutes of non-face-to-face care from the physicians. This includes phone check-ins, medication reviews, lab result discussions or other important health-related conversations. Providers use CCM CPT codes to track the time and bill for the services provided.
The CCM workflow in a health practice ensured consistent support to promote better health outcomes for patients. Subsequently, they enhance operational efficiency in the clinics and enhance reimbursement levels through Medicare.
What Are the Benefits of CCM for Patients and Providers?
Chronic Care Management aims to make healthcare and chronic disease care a win-win situation for patients and providers in modern healthcare. It provides tangible value in the following terms.
For Patients
- Continuous Care- Patients should not wait for the next physical appointment to get answers or help. CCM provides patients with constant care and support and 24/7 access to care professionals.
- Enhanced Quality of Life- With CCM, patients stay on top of medications and lifestyle alterations, which promotes better symptom control and improved daily functioning.
- Lesser ER Visits- Through a preventive approach, CCM ensures early interventions and avoids complications, which leads to fewer ER visits.
For Providers
- Versatile Revenue Stream- CCM is a Medicare-billed service extremely beneficial to patients. With CCM, providers can earn around $62 per patient monthly. More enrolled patients mean a higher revenue stream for providers.
- Informed and Happier Patients- Monthly interactions and continued virtual care mean educated patients, improved results, and enhanced patient satisfaction.
- Improved Healthcare Outcomes– Providers can utilise CCM to reduce care fragmentation and address red flags in the initial stages. This helps enhance clinical results amongst patients, which contributes to increased ratings and feedback for the provider.
What Services Are Included in CCM?
Patients with chronic conditions can expect several life-changing and health-enhancing services upon signing up for the CCM program. These services are designed to manage their health through preventive measures and reduce complications or emergency health situations. Key services include-
- Customized Care Planning: Providers carefully analyze factors like patients’ medical history, treatment goals, health status, preferences, and others to form a personalized care plan. Creating it once isn’t enough, and thus, providers regularly review and update the plan to ensure the patient’s evolving needs are met.
- Medication Reconciliation and Management: The care team monitors medications to ensure they are accurate, updated, and working without side effects or harmful interactions. The care team offers constant support to the patients to promote medication adherence and resolve persistent issues, if any.
- Coordination with Specialists: Providers, patients, and specialists work in sync under a chronic care management plan. Through seamless communication, which is properly documented, providers and specialists work together to devise the perfect care plan while minimizing duplication of tests or cases of care fragmentation.
- Preventive Care: The core focus of CCM lies in preventive and proactive care. Providers remind patients about preventive screenings or tests and vaccinations. Regular notifications about follow-up appointments help improve compliance with healthcare guidelines and enhance overall health results.
- Patient Education: CCM empowers patients to learn about health factors and manage specific chronic conditions. Through lifestyle modifications, coping strategies, and proper medications, patients are motivated to take an active role in maintaining good health and dealing with chronic conditions.
- Secure Messaging and Follow-ups: Addressing patients’ privacy concerns is an important part of CCM. Thus, care teams regularly connect with patients via secure messaging to keep their health information safe and meet their privacy requirements. Care providers also connect with patients through apps or phone calls to check their vitals and symptoms, review lab results, and provide reassurance and empathy. These interactions form the core of the billable virtual care time.
How Is CCM Different from Remote Patient Monitoring (RPM)?
Consider Remote Patient Monitoring an essential part of Chronic Care Management. RPM helps track the vitals of patients with chronic conditions regularly. Care providers analyze the vitals to check progress and alter the therapy and treatment plan if required. RPM is extremely helpful in conditions like hypertension, diabetes, and more, where tracking vitals like blood pressure or blood glucose level is quintessential almost every day.
CCM, on the contrary, is an amalgamation of different techniques such as RPM, RTM, MTM (Medication Therapy Management,) and more, focused on improving the overall health of the patient.
Here’s a detailed chart explaining the differences between CCM and RPM.
| Feature | CCM | RPM |
|---|---|---|
| Focus | Care coordination | Vital sign tracking |
| Patient Qualification | ≥2 chronic conditions | One chronic/acute condition |
| Reimbursement | Monthly | Daily |
| Device Requirement | No | Yes |
| Data Collection | Subjective/clinical | Objective/vital signs |
What Are the Medicare Requirements for CCM?
The CMS has devised a criterion to ensure quality and consistency in offering care to patients with multiple chronic conditions. This ensures a standardized program and offers dedicated and coordinated care to the best-suited beneficiaries. Here are the key Medicare requirements-
- Consent- Providers must obtain either written or verbal consent before initiating CCM services. This consent must cover details of the CCM therapy, including cost-sharing and the option to opt out at any time.
- 20 Minutes of Clinical Staff Time Monthly- Providers are obliged to offer a minimum of 20 minutes of non-face-to-face care management to patients according to calendar month. Physicians or other qualified healthcare professionals must talk to the patients and offer them guidance and counseling during this period.
- Certified Electronic Health Record- Physicians must create and document a comprehensive care plan with a certified electronic health record (EHR) system. The documented plan must include the patient’s medical history and functional and psychological needs. It must also outline measurable treatment goals and future plans.
- Round-the-clock Access- Patients must receive 24/7 access to care management services. An authorized and capable person must be available to address urgent care needs, resolve doubts, or provide support at any time of the day or night. This ensures continuity and coordination of care.
- Using EHR for Sharing Plans- All members of the care team and the patient must have access to the care plan and other important clinical information via a certified EHR. This promotes seamless communication and decision-making among all care professionals involved in the care plan.
How Can Providers Enroll and Bill for CCM Services?
For best results, providers must undertake structured implementation of CCM. The four steps, beginning from identifying eligible patients to justifiable billing, are mentioned below.
- Identifying Eligible Patients- Providers must ensure that the patient has two or more chronic conditions expected to last 12 months or till the patient’s death. Moreover, the conditions must pose a significant risk of death or functional decline. The providers are free to define eligibility based on these factors.
- Getting Consent from Patients- Before enrolling patients in a CCM program, providers should explain the program and its benefits and associated costs, if any. Once they understand and agree to be a part of the program, providers must record their consent in a verbal or oral form and add it to the medical record.
- Creating a Care Plan with Documentation- The next step is to document patient history, requirements, diagnosis, and the complete treatment communication. Based on this information, the providers create a comprehensive care plan that has to be updated within a certified EHR.
- Tracking Monthly Time Spent- Over the care period, the clinical staff must log the time spent on various CCM activities. Accurate time tracking helps meet Chronic Care Management requirements and receive adequate reimbursement.
- Billing for CCM Services- Using various Current Procedural Terminology (CPT) codes, staff can bill CCM services under Medicare Part B. Providers must ensure that documentation supports the billed time and services. More details about the CPT codes and CCM billing are explained in the next section.
What CPT Codes Are Used for CCM Billing in 2025?
Here’s a table illustrating the CPT codes used for billing CCM services, along with a brief description of the service and the reimbursement.
| CPT Code | Description | Reimbursement* |
|---|---|---|
| 99490 | 20 minutes of CCM services by clinical staff | $64 |
| 99439 | Each additional 20 minutes | $48 |
| 99491 | CCM services by a physician or other QHP | $85 |
| 99437 | An additional 30 minutes by physician/QHP | $60 |
What Are the Documentation Requirements for CCM?
A successful CCM program demands accurate and compliant documentation. The CMS requires detailed records to offer proper reimbursement, and failure to document clearly can cause denied claims, unwanted audits, or even penalties. Parts of CCM that require proper documentation include-
- Patient Consent- Before initiating CCM services, it is vital for providers to document patient consent. This must include patient understanding and agreement regarding CCM services and potential co-pays.
- Care Plan- A certified Electronic Health Record must store a comprehensive care plan focusing on the patient’s personalised needs. It must have measurable treatment benchmarks and other important treatment factors such as medication management, lifestyle changes, etc.
- Date and Time of Interactions- All CCM activities, such as virtual interactions and online consultations, must be timestamped. A complete record enhances transparency and makes the reimbursement process easy. Interactions such as phone calls, lab report reviews, and other patient-related tasks must be properly recorded.
- Time Spent on CCM Activities- CCM makes it compulsory for providers to offer and track at least 20 minutes of clinical staff time to each patient monthly. Providers should maintain a track of the time spent on CCM activities each month for general CCM billing (CPT 99490) and higher-tier codes for additional time.
- Summary of Actions- Physicians must include a brief description of actions taken during the recorded time in each entry. Tasks such as medication reconciliation, referral,s or follow-ups must be summarized in each entry.
Clear documentation enables providers to offer transparent and compliant Chronic Care Management services to patients.
How Can Technology Support Chronic Care Management?
Manual implementation of CCM is a time-consuming process that can overburden your staff and have adverse impacts on your practice. Technological advancements can be used to streamline the process and make the transition to CCM easier. Here’s how technology solutions can help you-
- Workflow Automation- Technology can take up repetitive tasks such as patient outreach, reminders, and scheduling, etc, to eliminate unwanted burden from the staff’s shoulders.
- Accurate Time Tracking- Equipment can help you automatically log and calculate the time spent on each service in the case of each patient. This can help you track services and bill accurately.
- Integration with EHRs- With the help of technology, providers can store and update care plans in existing EHRs. This allows documenting patient interactions in real-time seamless.
- Simplified Billing and Reporting- By helping you generate automatic CPT coding and billing reports, technology helps reduce administrative burden and improve care efficiency.
HealthArc offers a powerful EHR-integrated CCM solution that helps providers track clinical time spent on each patient seamlessly. By automating care plan creation and integrating with RPM and other care management tools, it ensures HIPAA compliance and helps small care practices scale and operate smoothly.
Common Technologies Used in Chronic Care Management
CCM uses multiple technologies to improve patient outcomes through constant monitoring and support. These technologies help reduce staff workload, enhance efficiency and ensure accuracy of documentation and timestamping. Let’s take a detailed look at the technologies used in CCM-
- Remote Patient Monitoring: Monitoring patient vitals is a quintessential part of Chronic Care Management, especially in cases of diabetes, hypertension, and heart failure. Here are some key devices/technologies used in Remote Patient Monitoring (RPM).
-
- Wearable Devices- Providers use smartwatches or fitness trackers to collect data such as activity levels, vital signs, sleep patterns, heart rate, and more to monitor patients continuously.
- Specialized Devices- Certified health devices such as glucometers, blood pressure monitors, and respiratory monitors are also used to track health metrics.
- Data Transmission- Physicians ensure these devices are capable of data transmission. This enables the accuracy of data so that patients do not have to self-report.
- Electronic Health Records (EHRs): EHRs are a database of patient health information such as medical history, test results, and treatment plans etc. They facilitate data sharing among care providers, physicians, patients, and other stakeholders. Through EHRs, patients get access to their health information, which motivates them to participate in their wellness regime actively.
- Artificial Intelligence and Data Analytics: A well-set-up CCM system consists of AI algorithms that analyze patient data to identify issues, predict health risks, and catch complications in their initial phase. Additionally, providers can leverage AI to create customized treatment plans based on individual patient needs and preferences.
AI can automate monotonous and time-consuming tasks such as sending medication and follow-up reminders, scheduling appointments, and documentation. AI-powered chatbots can be utilized to offer continuous support and care to CCM beneficiaries. Chatbots can answer their questions, inform them about their conditions, and offer support while reducing human tasks.
- Telehealth: CCM focuses on virtual care and telehealth platforms that make that possible. By enabling virtual doctor consultations and connecting patients with doctors through the comforts of their home, telehealth tools facilitate CCM. Providers link telehealth systems with RPM devices, enabling physicians to access patient data in real-time. Through technology, telehealth promotes access to care in remote or underserved areas.
- Cloud-Based Platforms: Privacy concerns often hover patients’ minds while sharing sensitive data with providers. To address these issues, providers must use secure cloud-based platforms for storing patient information without the fear of data theft. It also enables real-time update sharing so that patients can track their health and physicians can make informed decisions with accurate information.
- Reporting Tools: Tools for documentation and reporting play a major role in chronic care management. Reporting tools play a major role in identifying negative trends in patient health data and spotting complexities if any complexities. Moreover, the transparency of reporting tools ensures that patients are engaged in the process of improving their health outcomes using CCM.
- Mobile Health (mHealth): Apps and software on mobile phones form an integral part of CCM nowadays. By offering insights into bodily trends, tracking medications, and providing instant communication with providers, these technologies help patients manage their health.
Using these tools helps providers and small practiced prevent burnout while handling more patients with fewer tasks involved. In the long run, these tools help improve operational efficiency and enhance reimbursement. Moreover, these tools make complying with the rules quite easy.
Also read- Chronic Care Management Trends 2025: CMS Updates, AI Tools & RPM Integration
What Challenges Do Providers Face in Implementing CCM?
CCM holds great promise for the care industry. However, many providers experience operational and practical challenges during the implementation phase. Common roadblocks include-
- Staffing Limitations- Implementation of CCM demands dedicated and skilled clinical staff for delivering CCM services. Many small and medium care practices lack the staff and are unable to meet the staffing demands of CCM.
- Integration with Existing EHRs- Documentation and communication can be a challenge in poorly integrated platforms. Many small providers experience difficulty in integrating the CCM workflow with existing electronic health records.
- Patient Engagement- Keeping the patient engaged and responsive during virtual interactions is a challenge, especially in the case of elderly patients. The staff needs to be well-trained, and the patients must be well-informed and educated to allow a responsive treatment plan.
- Accuracy of Time-Tracking- Manual time tracking is erroneous, and every care episode isn’t properly documented without the help of technology. Providers who fail to integrate time-tracking equipment often face increased inconsistencies and reimbursement issues.
- Documentation Compliance- Documentation is key in CCM services, and ensuring every care episode is aptly documented increases administrative burden for small practices.
These challenges seem daunting, but can be tackled with important investments that come along with CCM integration. With apt staff training and by embedding technology infrastructure, small care providers can seamlessly implement Chronic Care Management into their practice. CCM integration also demands continuous process optimization to ensure everything operates smoothly.
How Can HealthArc Help with Chronic Care Management Services?
HealthArc makes CCM integration a cakewalk for small practices. With our solutions, you can address administrative and clinical needs to make CCM effective, compliant, and profitable.
Our secure and cloud-based HIPAA-compliant platform makes adherence to rules easy for you. Our workflows are compatible with major EHR systems to make integration smooth for your ongoing processes. Additionally, we provide training and ongoing support after dedicated onboarding to guide your staff at every step.
At HealthArc, we believe in the power of customization. Thus, our tools enable providers to create patient-centric care plans. With automated CPT codes and billing, we also make claims submission and faster reimbursements easy for you.
Case Study
In early 2023, Sunrise Family Clinic, a small primary care practice in Texas, joined hands with HealthArc to integrate and launch CCM into their array of care services. Within 6 months, they successfully enrolled over 250 patients and generated an additional $40,000 in Medicare revenue. Apart from this, they witnessed a 23% increase in patient satisfaction scores and a 17% decrease in emergency visits or hospital readmissions.
This case highlights the power of a well-implemented CCM program with the right technology. With the support of HealthArc, you can improve financial outcomes and the quality of care and engagement offered to the patients.
Key Takeaways
- 24/7 virtual care for patients with multiple Chronic Conditions.
- Medicare reimbursements up to $62/patient/month for providers.
- 15% fewer hospitalizations for CCM participants.
- $40,000 added Medicare revenue in 6 months (case study).
- Tech‑enabled efficiency with EHRs, RPM, and AI tools.
- $74 annual savings/patient and 20% cost reduction over 2 years (CMS).
Conclusion
The United States fosters a healthcare environment based on the principles of value-based care. Given the current needs and the condition of patients with chronic ailments, Chronic Care Management is more than a program– it’s a necessity. CCM offers care beyond the clinic walls and helps motivate and engage patients in maintaining their well-being. Additionally, it serves as an exceptional and stabilized revenue stream for small providers.
If your clinic is looking to improve patient outcomes, expand the scope of care services, and get additional reimbursement, now is the time to integrate CCM into your clinic. With the help of trusted platforms like HealthArc, you can seamlessly implement Chronic Care Management and make the most of the CMS reimbursement structure.
Frequently Asked Questions (FAQs)
In the 1990s, Dr. Edward H. Wagner and his team developed the Chronic Care model to improve chronic illness management by initiating a more proactive and patient-centred care approach. Medicare introduced the Chronic Care Management system in January 2015 to compensate providers for virtual care services offered to patients with multiple chronic problems.
CCM stands for Chronic Care Management. It includes the set of services offered to patients with chronic illnesses to help manage their therapies and treatment.
Common CPT codes used for billing for CCM services include CPT 99490, CPT 99439, CPT 99491, and CPT 99437.
Chronic Care Management and Principal Care Management are both care coordination services. However, CCM is for patients with two or more chronic conditions expected to last 12 months or for a lifetime, and PCM is for patients with one complex condition expected to last at least 3 months.
Key technologies used in providing CCM services include Electronic Health Records, Time-Tracking Software, Patient Engagement Tools, Remote Patient Monitoring (RPM) devices, and Automated Billing Platforms.
If you are looking to broaden the scope of your care services, you can integrate CCM in your clinic with the help of HealthArc. Our solutions are easy to embed and use, and our expert team can streamline setup, documentation, and billing for your clinic. We also offer continued support and training for your staff till you get well-versed with the technologies.
The six elements of the Chronic Care Model are self-management, decision support, community resources, clinical information systems, health care organization, and delivery system design.
Steps involved in Chronic Care Management include assessment, care planning, patient education and consent, time-tracking, documentation, and compliance.
Bibliography
- HealthArc. (n.d.). Chronic Care Management (CCM) platform. Retrieved July 26, 2025,
- HealthSnap. (n.d.). CCM 101: What is Chronic Care Management?. Retrieved July 26, 2025,
- WebMD. (n.d.). What is chronic care management? Retrieved July 26, 2025,
- Centers for Disease Control and Prevention. (n.d.). Chronic disease overview. CDC.
- Centers for Medicare & Medicaid Services. (2022). Chronic care management services.
- Market.us. (2024). Chronic care management statistics – Benefits, cost, and implementation.
Most Recent Blogs
Categories
Related Blog
- February 3, 2026 | Read Time: 17 mins
Prevention in Health Care: Why Preventive Care Is Becoming a Connected, Continuous Model (RPM, CCM, BHI, APCM and More)
People typically associate health care prevention with their annual physical exams and...
Learn More- January 14, 2026 | Read Time: 12 mins
What Is a Care Manager? Roles and Responsibilities
A care manager is a dedicated healthcare professional who helps patients navigate...
Learn More


