A Complete Guide to Remote Patient Monitoring (RPM)

The rapid growth of digital technology has gone a long way toward defining modern healthcare, allowing innovative models of patient care to form. Amidst these advancements, Remote Patient Monitoring (RPM) has established itself as a key aspect of value-based care. RPM employs connected devices and cloud-based platforms to continuously monitor patients outside of traditional clinical settings. This real-time patient monitoring allows healthcare providers to collect, analyze, and act on patient data while proactively monitoring patients and eliminating unnecessary hospital visits.
The COVID-19 pandemic accelerated RPM adoption and it has continuously delivered tremendous value for patients managing chronic conditions, the elderly, and those recovering from surgical procedures, allowing for real-time monitoring that facilitate timely interventions and patient-centered care.
Public policy has supported the movement toward RPM and care models that more proactively support patient needs beyond the clinical setting, especially as groups like the Centers for Medicare & Medicaid Services (CMS) expanded reimbursement for RPM services. As such, RPM has evolved beyond a trend in healthcare and established a strong foundation in patient-centered, technology-driven care.
This blog explains RPM components, how CPT billing codes work, and emerging trends, so providers can implement them effectively.
Table of Contents
ToggleWhat Is Remote Patient Monitoring?
Remote Patient Monitoring (RPM) is a form of telehealth program that utilizes technology to collect health data from patients in one location and send it to healthcare providers in another. The goal of RPM is to improve the value of care by allowing monitoring in real time or remotely, outside of the clinical settings, most often in the patient’s home. RPM works to collect metrics of multiple physiological variables using digital FDA-approved devices that monitor vitals, such as:
- Blood pressure
- Heart rate
- Glucose
- Blood oxygen saturation (SpO2)
- Weight
- Temperature
- Respiratory rate
The patient’s health data is transmitted to a healthcare team through a secure cloud-based platform. Multiple providers can work in conjunction with algorithms using artificial intelligence (AI) and machine learning, which are trained to flag anomalies and create actionable insights.
Key features of RPM include:
- Continuous monitoring: Unlike assessments that occur only during a clinic visit, RPM is continuous, daily, even hourly.
- Preventive strategy: RPM identifies early signs of deterioration, allowing for intervention before hospital visits are required.
- Patient involvement: Patients are involved in their care by having their data monitored.
The benefits of RPM are not only convenience, but they also lead to improved clinical outcomes, improved care satisfaction, and lighten the load on already overwhelmed health systems.
What Is the Purpose of Remote Patient Monitoring?
The key strength of Remote Patient Monitoring is that it offers an efficient way to provide oversight of a patient’s health condition while narrowing the gap between in-person visits and self-care. RPM is especially beneficial for chronic disease management, post-acute care, and managing higher-risk populations.
| Purpose of Remote Patient Monitoring (RPM) | Explanation |
|---|---|
| Chronic Disease Management | RPM is effective for chronic diseases such as hypertension, diabetes, heart failure, chronic obstructive pulmonary disease (COPD), and other chronic illnesses. Advances in technology now enable clinicians to make alterations to treatment plans in real time and adjust medications before complications arise. |
| Prevention of Hospital Re-admissions | RPM allows clinicians to intervene more quickly to prevent a patient from returning to the hospital. This is the most common quality metric and is valuable for clinicians to consider during the 30 days after discharge, since hospitals are penalized with decreased Medicare reimbursement via CMS for re-admissions. |
| Increasing Preventive Care | RPM allows clinicians to intervene when early warning signs such as high glucose levels or abnormal heart rhythms appear. This process reduces disease prevalence and even saves money in the healthcare system. |
| Patients Are No Longer Passive Participants in Their Care | RPM encourages patients to be more engaged, thus promoting self-awareness, medication adherence, and health literacy. RPM not only emphasizes all the principles discussed thus far at an individual level, but also leverages the interactive framework of the RPM platform, which includes feedback loops, education, and virtual coaching. |
| Advocating for Value-Based Care | RPM aligns with value-based care models that reward better outcomes, not the sheer volume of services. RPM can provide measurable metrics to demonstrate improved quality, population health management, and cost containment. |
| Providing Equitable Access to Care | For patients in rural or under served locations, RPM provides access to near-continuous care without the burden of traveling long distances. This addresses inequities and promotes the improvement of population health metrics. |
In conclusion, RPM is more than just a monitoring program that paves the way for proactive, equitable, and efficient health management.
What are the Components of Remote Patient Monitoring
| Component | Description |
|---|---|
| Remote Monitoring Devices | Remote monitoring devices are the first point of contact with the patient’s data. Devices vary depending on the condition and target of monitoring. For example: • Blood pressure monitors: to monitor patients with hypertension and heart disease. • Glucose meters: for monitoring patients with diabetes. • Pulse oximeters: for monitoring blood oxygen levels; can be helpful with COVID-19 patients and patients with COPD. • Weight scales: for patients with heart failure. • ECG devices: for monitoring heart rhythms. • Smart thermometers: for monitoring trends in body temperature data.All devices used need to be FDA-approved and able to securely transmit the data. |
| Connectivity and Communication Networks | RPM devices can send patient data via: • Bluetooth: common for patient monitoring and short-range communication with mobile apps. • Cellular networks: good for patients who do not have internet at home. • Wi-Fi: provides faster upload of data via better connectivity. • IoT-enabled devices: work in tandem with any smart home technology to improve access to patient data and enhance the experience.To maintain security, data is typically encrypted in a manner consistent with HIPAA standards. |
| Patient Portal or Mobile Application | Patients are typically exposed to RPM via an app or portal. The interface allows: • Visualizing their health trends • Messaging or alerts • Completion of health questionnaires • Scheduling reminders for medication and testsApps will also frequently offer educational materials, chat support, and feedback options. |
| Clinical Dashboard for Providers | Clinicians have a single dashboard for reviewing: • Patient trends • AI-generated alerts • Adjustments to care plans • Patient engagementModern dashboards allow customization, prioritization of high-risk patients, and seamless access from Electronic Health Records (EHRs). |
| Data Analytics & Decision Support | AI & ML algorithms analyze large quantities of incoming data to reveal trends, flag anomalies, and provide predictive suggestions. They can do things like: • Determine medication side effects • Indicate emergencies • Suggest adjustments to care plans |
| Electronic Health Records Integration | Integrated Electronic Health Records allow for RPM data to be included in the patient’s longitudinal health record. This allows better care coordination and compliance with documentation standards. |
| Support and Training Infrastructure | RPM onboarding and support are key factors for successful RPM implementation. Teaching patients how to use devices and read their data is part of the connectivity. It is important for patients to know how to respond to alerts. Likewise, providers must be onboarded to their dashboards, billing, and compliance. |
To conclude, RPM requires a number of sophisticated components: medical-grade devices, secure data transmission, patient engagement platforms, and clinical dashboards, working together around the goal of enhanced care delivery.
Types of RPM Devices That Simplify Patient Monitoring
There are a variety of different RPM devices to collect patient data. For patient safety, accuracy, and reimbursements, it is important RPM devices be cleared or approved by the FDA. Most 510(k) devices are cleared under the FDA’s 510(k) clearance process that denotes the device is substantially equivalent to a legally marketed device. This clearance also makes the device eligible for CMS reimbursement under RPM specific CPT codes. The most commonly used devices include:
| Device | Description |
|---|---|
 1. Blood Pressure Monitors |
Used for managing hypertension and cardiovascular disease, blood pressure monitors allow for reliable monitoring that can lead to early intervention prior to emergencies. |
 2. Glucometers |
Glucometers are essential to managing diabetes. CGM or Continuous Glucose Monitor provides the patient with their glucose levels in real-time. |
 3. Pulse Oximeters |
Pulse oximeters measure oxygen saturation. They are useful in the management of COPD or during recovery from respiratory illnesses. |
 4. Smart Scales |
Smart scales track fluid retention and weight changes. They are useful in managing heart failure and obesity. |
 5. Wearable ECG Monitors |
Monitors that continuously assess the electrical activity of the heart can provide early detection of arrhythmias (such as atrial fibrillation). This type of monitoring enables continuous cardiac monitoring. |
 6. Thermometers |
Useful to monitor infection and fluctuating body temperature post-op. |
7. Spirometers |
Used to monitor lung function in asthma and COPD patients. |
 8. Wearables (watches) |
Monitoring heart rate, activity, and sleep patterns enable both the preventative and chronic care model to be adopted. |
9. Medication Adherence Tools |
Smart dispensers or notification systems can help reduce missed medications doses. |
 10. Multi-parameter Devices |
Devices that have different sensors combined into one device (e.g. BP, HR, SpO₂, temperature) and are useful for patients with complex medical conditions. |
Most of the devices listed above come complete with the ability to sync to smartphones via Bluetooth or cellular signals, graft patients onto EHRs, and supply patients with a mobile app to ensure data is easily transmitted and flowed between the patients and providers.
What Are RPM Platforms?
Remote Patient Monitoring (RPM) platforms are varied digital health platforms that enable clinicians to monitor their patients in the home setting. They serve as a connection point between patients, clinicians, and relevant health data in real-time.
RPM platforms utilize FDA approved medical devices and software where clinicians can establish reporting on patients’ vital signs. For example, RPM platforms have software applications for monitoring blood pressures in a hypertension patient or blood glucose levels in a diabetic patient. Next, we will take a closer look at RPM platforms and the impact they have on patient engagement:
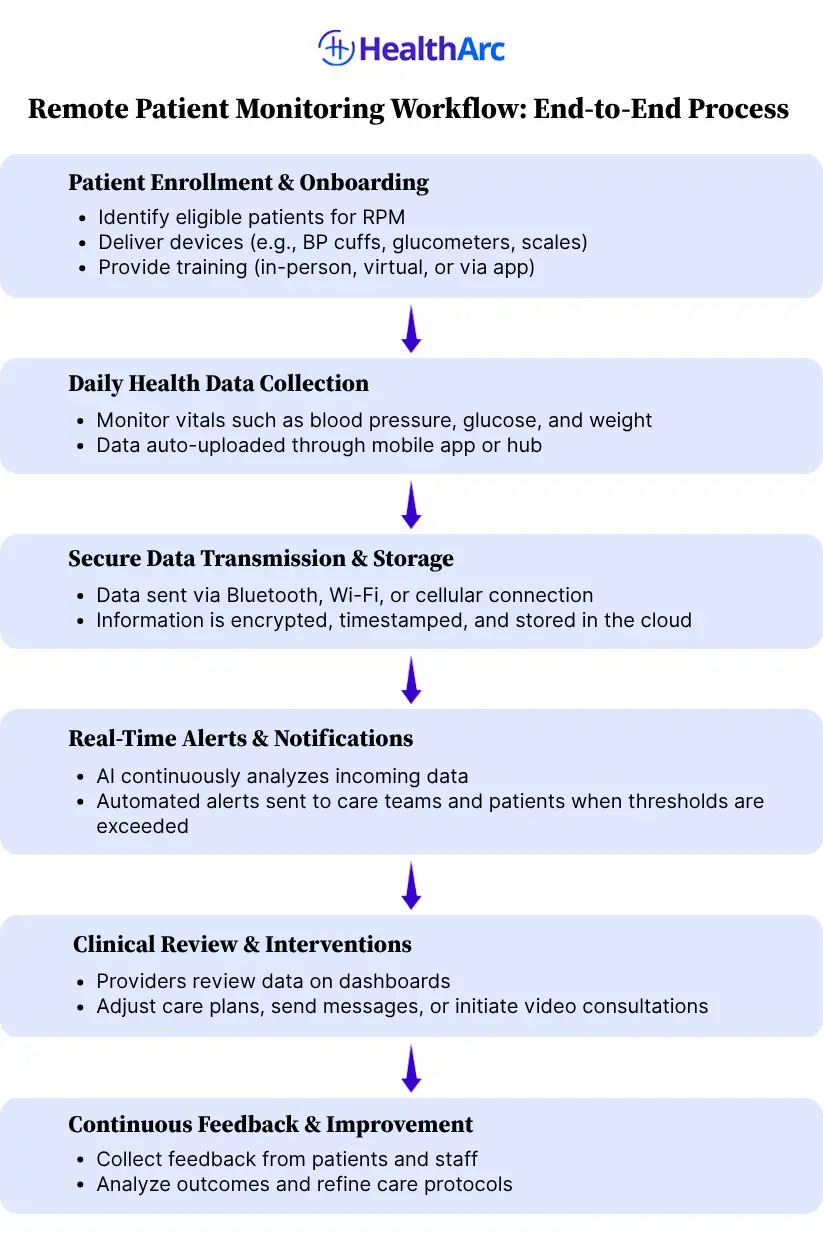
- Patient Enrollment & Onboarding: The RPM journey begins with the identification of eligible patients, generally those managing a chronic illness, such as hypertension, diabetes, Chronic Obstructive Pulmonary Disease (COPD), or those recently discharged from an inpatient hospital setting, since these patients are “high-risk” patients who will benefit significantly from remote monitoring at home. RPM patients can be enrolled and onboarded from clinician referral, use of algorithms from population health, or during transitions of care.
- Daily Vital Sign Collection: Once patients are enrolled and set up, they start to use their devices to monitor important vitals. The parameters, to name a few, include blood pressure, blood glucose, oxygen saturation (SpO₂), weight, heart rate, and sometimes, the respiratory rate or ECG rhythms. The ease of use is an important consideration. The devices are Bluetooth-enabled, directly connecting to an app or home gateway device automatically. Some also use cellular transmission built into each device, which eliminates the need for Wi-Fi access in the home and creates more access for at-home monitoring.
- Secure Data Transmission & Storage: Data security is a foundation of all RPM platforms. Patient health information (PHI) needs to be encrypted in storage and in transfer to satisfy HIPAA guidelines. Once the data is captured via the RPM device, it transfers to secure networks in real time for storage. Each reading is automatically marked with the date and time, tagged, and laid out in an organized way.
- Real-Time Alerts & Notifications: Arguably the most important aspect of RPM platforms is their ability to produce real-time alerts around clinical thresholds. These thresholds are either set or programmed based on clinical guidelines or customized for a certain patient. If a reading passes above threshold or drops below threshold, an automated alert is shared with the clinical care team. Patients may receive an automated app alert with self-care advice or prompts for follow up.
- Clinical Review & Interventions: While AI and automated alerts provide the core of the RPM platforms, there is still a necessary human role. Clinicians interact with an intuitive provider dashboard to see individual readings, track trends, and prioritize patients needing intervention. Clinicians are also able to send secure messages with the patient from the dashboard, change care plans, and schedule follow-ups. Most RPM platforms build in the ability to also link documentation to an EHR (Electronic Health Record) system.
- Automated Documentation & Billing: RPM platforms are also designed to assist healthcare organizations with billing and compliance. Every patient interaction, device reading, and minute spent reviewing against the clinical thresholds is documented automatically. This documentation aligns with the requirements and allows billing for certain Medicare CPT Codes:
- 99453 for setup and patient education
- 99454 for device data transmission and monitoring
- 99457/99458 for time spent reviewing and interacting with patients
RPM platforms are streamlining the documentation process and are reducing administrative challenges for providers and their billing departments. This increases revenue potential and maintains compliance with CMS requirements that are necessary for program sustainability.
- Continuous Feedback & Care Optimization: RPM platforms do more than simply collecting data and responding to it, they also give feedback on patient engagement, clinical outcomes, and adherence. Providers can see which patients regularly stay in compliance, which is dropping off, and what interventions are being implemented. This creates a continuous data/feedback loop that allows for care optimization. Treatment plans can move and be adjusted dynamically, based on what the patient is actually doing and what results have been achieved.
How Does RPM Work?
Benefits of Remote Patient Monitoring (RPM)
Top Benefits of RPM for Healthcare Providers
| Benefit | Description |
|---|---|
| Better Clinical Outcomes | 24/7 monitoring enables early intervention, personalized care plans, and real-time clinical decisions. |
| Reduction of ER Utilization and Hospital Readmissions | RPM helps reduce readmissions, especially post-discharge, avoiding CMS penalties. |
| Improved Workflow Efficiency | Automated alerts and data collection let care teams focus on critical interventions. |
| New Billing Opportunities | Reimbursement available through CPT codes (99453, 99454, 99457, 99458) increases revenue potential. |
| Aligned with Value-Based Care | Supports KPIs like reduced ER visits and better chronic disease management. |
| Improved Patient Engagement and Adherence | Video guides and reminders enhance adherence to treatment plans. |
| Real-Time Data Insights | Trends and predictive analytics support better diagnoses and proactive care. |
| Expanded Reach and Scalability | Enables monitoring of more patients without requiring more staff, ideal for rural/underserved regions. |
| Integration with EHRs | Seamless EHR integration improves data continuity and care coordination. |
| Competitive Advantage | Positions providers as innovative leaders using tech-savvy care models. |
Top Benefits of RPM for Patients
| Benefit | Description |
|---|---|
| Continuous Health Monitoring | Ongoing tracking of vitals offers peace of mind and clinical awareness. |
| Earlier Detection of Health Issues | Enables early treatment through real-time alerts. |
| Convenience of RPM | Patients can measure vitals from home, improving access for elderly/rural individuals. |
| Focused Attention on Your Care | Personalized treatment plans improve outcomes and satisfaction. |
| Better Health Literacy | Educational content helps patients understand and manage their health. |
| Better Communication with Providers | Secure messaging and telehealth allow quicker, easier communication. |
| Promotion of Healthy Behaviors | Daily monitoring encourages medication, diet, and exercise adherence. |
| Decreased Hospitalizations and ER Visits | Fewer emergency situations due to proactive intervention. |
| Cost Savings | Reduced need for ER visits and long hospital stays lowers costs. |
| Improved Satisfaction and Trust | Patients feel more in control and connected with providers. |
Comparison: RPM vs. Other Remote Health Monitoring Programs
Faced with multiple remote health monitoring solutions, Remote Patient Monitoring (RPM) is the best choice among digital health solutions because of conclusive evidence of better health outcomes, a comprehensive reimbursement structure, and its capacity to engage care at scale with patient populations.
Below is a comparison table highlighting the advantages of RPM over other remote health monitoring programs:
| Advantage Area | Remote Patient Monitoring (RPM) | Other Remote Health Monitoring Programs |
|---|---|---|
| 1. Reimbursement Support | Reimbursement-Driven and Backed by CMS with established CPT codes. | Wellness apps or telehealth often lack long-term reimbursement models. |
| 2. Clinical vs. Lifestyle Focus | Clinical Monitoring Focused – uses FDA-approved devices for data-driven decisions. | Often limited to lifestyle engagement via fitness trackers or wellness apps. |
| 3. Chronic Care Coordination | Works in tandem with CCM for chronic care documentation and outcome improvement. | Limited capability to coordinate care or support chronic conditions. |
| 4. Value-Based Care Alignment | High adoption among ACOs and Medicare Advantage for meeting quality metrics. | Less aligned with value-based care and performance tracking. |
| 5. Real-Time Insights | Provides real-time, actionable data for proactive clinical interventions. | Typically provides delayed or aggregate data. |
| 6. Regulatory Compliance | Meets FDA standards and clinical regulatory thresholds. | Less regulated; may not meet clinical-grade standards. |
| 7. Patient Trust & Engagement | Device prescribed by a clinician with direct feedback builds trust and engagement. | Self-managed apps often suffer from low long-term engagement. |
| 8. Population Health Enablement | Enables large-scale monitoring, risk stratification, and nursing alerts. | Limited in stratifying risks or reaching broad patient populations. |
| 9. EHR Integration | Fully integrates with EHRs for seamless workflows, documentation, and billing. | Often operates separately without EMR integration. |
| 10. Scalability | Cloud-based and scalable without major infrastructure investment. | Usually not scalable beyond basic app or device capabilities. |
Eligibility Criteria
RPM Eligibility Criteria for Patients
A. General Requirements
- Must be a Medicare beneficiary or a patient under some private insurances.
- Patient or legal guardian must consent to RPM services (verbal or written consent is acceptable, but must be documented in the medical record).
- RPM services must be ordered by a qualified healthcare provider and be part of the patient’s treatment plan.
- RPM services must be medically necessary.
________________________________________
B. Clinical Requirements
- Patient suffering from chronic conditions that require constant monitoring. RPM generally helps with the management of conditions such as:
- Hypertension
- Diabetes
- Heart failure
- COPD
- Asthma
- Obesity
- Kidney disease
- Patients suffering from acute conditions that are quite complex to be monitored and needs prolonged care and management, such as:
- Post-surgical recovery
- COVID-19
- Pneumonia
- Infections
- Patient attributes that signify RPM eligibility include:
- Experiencing one or more chronic conditions
- Need to monitor vitals on a regular basis
- Experiencing trouble visiting clinics regularly
- Have been admitted to a hospital or visited an emergency room in the past
- An increased risk for complications without being monitored continuously
________________________________________
RPM Eligibility Criteria for Healthcare Providers
A. General Requirements
Only Medicare-eligible providers who are authorized to bill Evaluation and Management (E/M) services can order and bill for RPM, including Physicians (MD/DO), Nurse Practitioners (NPs), Physician Assistants (PAs), Clinical Nurse Specialists (CNSs), and Certified Nurse Midwives (CNMs).
B. Supervision Requirements
RPM services can be delivered under general supervision, meaning the supervising provider does not need to be physically present. Clinical staff (e.g., nurses, MAs) may help monitor and communicate with patients as long as a qualified provider oversees and bills for the service.
C. License Requirements
- Providers must be licensed in the state where the patient resides.
- Services must fall within the provider’s scope of practice as defined by state law.
- Telehealth laws may affect cross-state RPM provision.
D. Technology and Infrastructure Requirements
Providers must use FDA-defined medical devices capable of:
- Automatic, electronic transmission of patient data
- Secure, HIPAA-compliant RPM software
- Must have access to a HIPAA-compliant RPM platform or dashboard to store, analyze, and respond to incoming patient data.
Timeline for Remote Patient Monitoring Services
| Phase | Timeframe | Description | Key Activities |
|---|---|---|---|
| Phase 1: Assessment & Eligibility Review | Week 1 | Providers must determine the patient’s eligibility before they can offer RPM services. The patient’s medical history, diagnosis, and treatment requirements and objectives are the three components of this evaluation. | • Identify chronic/acute conditions • Verify insurance eligibility (Medicare/private) • Obtain patient consent • Select RPM technology based on care needs |
| Phase 2: Device Selection & Enrollment | Week 1–2 | The provider will choose a suitable RPM device once the patient’s eligibility status has been established. | • Order FDA-cleared RPM device (e.g., BP monitor, glucometer) • Enroll patient on platform (e.g., HealthArc) • Set up patient profile and data transfer • Train patient on device use |
| Phase 3: Initial Data Collection & Calibration | Weeks 2–3 | Begin capturing data and ensuring stable transmission | • Confirm accurate device pairing • Resolve connectivity issues • Educate patient for regular usage (≥16 days/month) • Set clinical thresholds for alerts |
| Phase 4: Active Monitoring and Clinical Review | Ongoing from Month 1 | Continuous review of health data and clinical response | • Daily review of patient data • Trigger alerts for abnormal values • Schedule/document telehealth check-ins • Record clinical interventions and notes |
| Phase 5: Monthly Reporting & Billing | End of Each Month | Validate compliance and submit reimbursement claims | • Verify 16-day minimum data for CPT 99454 • Compile monthly report • Submit billing claims (99453, 99454, 99457, 99458) • Update medical records and outcomes |
| Phase 6: Long-Term Continuity and Reassessment | Every 3–6 Months | Reevaluate RPM effectiveness and adjust care plans | • Review patient status and RPM necessity • Upgrade/replace devices if needed • Confirm ongoing patient engagement • Modify care plan based on progress |
The timeline for Remote Patient Monitoring is a continuum of events, from establishing eligibility to long-term care. Providers who engage in a standardized, systematic process will increase the likelihood of patient success, decrease hospitalizations, and maximize reimbursement.
- Develop consistent workflows for onboarding.
- Use automated alerts to minimize manual monitoring.
- Ensure patients have clear communication channels with your team.
- Consider a platform like HealthArc to manage workflows, care plans, alerts, and billing in one integrated experience.
RPM is not simply a technology being offered to patients; it is an evolving, revolutionary care model that leans toward continuous engagement and actionable information.
The Regulatory Environment For Compliance & Privacy Standards
The United States Food and Drug Administration (FDA) is an essential player in the design, approval, and post-marketing surveillance of Remote Patient Monitoring devices. Nowadays, many health organizations are practicing RPM and adhering to the FDA’s regulations is not only an obligation but also a commitment to patient safety, clinical accuracy, and your ability to bill on behalf of the work you do.
- Device Classification and FDA Clearance: RPM devices can be classified into several categories of medical devices by the FDA, all of which are classified in class I, class II, or class III. Many RPM devices, such as blood pressure cuffs, glucose meters, wearable ECG monitors, are classified as class II because they require a premarket notification (510(k) clearance) that demonstrates they are “substantially equivalent” to a previously legally marketed device and that have certain safety and performance standards.
- Cybersecurity Standards: Given that many RPM systems are transporting sensitive health data to cloud platforms or mobile applications, cybersecurity standards have become a regulatory priority as well. The FDA requires that manufacturers include cybersecurity in the design and development phases of the system to the point where the device includes encryption, secure firmware update process, user authentication, and measures to prevent unauthorized access to personal health information and manipulation of the devices.
- Quality System Regulation (QSR): The FDA implements the Quality System Regulation (21 CFR Part 820), which defines current Good Manufacturing Practices (cGMP) for medical devices. These manufacturers of RPM devices must establish and maintain a comprehensive quality system that controls the design and testing of the product, the manufacturing process, and corrective action, to ensure that every time they produce the device it is consistently reliable and safe.
- Post-Market Surveillance and Adverse Event Reporting: The RPM device will still go through continued regulatory scrutiny in the way of post-market surveillance protocols, even after obtaining FDA clearance. Manufacturers will be required to verify the device’s functionality, and if there were issues reported by users or adverse events associated with their device, they will have to communicate these to the FDA through the Medical Device Reporting (MDR) process. This creates a consistent flow of information from the manufacturer to the regulator, which is intended to allow both entities to respond in a timely manner to use and safety issues.
- Digital Health Software Precertification Program: To ensure that the rapid health technology digital ecosystem keeps evolving responsibly, the FDA created a Software Precertification Pilot Program, focused on the FDA’s Digital Health Innovation Action Plan. This program establishes a model relying on a company’s software development capabilities rather than reviewing individual products. The FDA has an interest in enabling manufacturer’s speed of entry into the markets with digital health tools, including RPM software, without sacrificing the safety for their consumers.
- Reimbursement Considerations: From a provider’s standpoint, utilizing RPM devices that have been cleared by the FDA is a necessary precondition to cover eligible Medicare RPM billing codes (e.g., CPT 99453, 99454, 99457, and 99458). Most commercial payers have similar restrictions. Providers should document all RPM hardware and software utilized in the care of their patients, including FDA clearance.
Documentation Required for CMS Remote Patient Monitoring (RPM)
| Requirement | Description |
|---|---|
| Documentation of Patient Consent | CMS mandates obtaining informed consent from patients before initiating RPM services. Patient consent can be verbal or written but should be documented in the medical record, and should include:
• A statement describing the RPM services. |
| Initial Patient Assessment and Eligibility | Documentation must include the medical necessity of RPM based on the patient’s condition, including: • Demographics • Chronic or acute conditions • Clinician’s rationale for RPM use. |
| Device Setup and Patient Education | CPT code 99453 covers device setup and onboarding. Documentation must include setup and training, including: • Date of device setup. • Type of device issued. • Type of training provided (in-person or remote). • Confirmation that the device was operational and understood by the patient. |
| Data Transmission & Monitoring Reports | To bill, data must be transmitted at least 16 times in 30 days using an FDA-cleared device and document: • Dates and times of data transmissions. • Types of vitals recorded (e.g., blood pressure, glucose). • Device logs or EHR-integrated usage. |
| Time Spent for RPM Services | CPT codes 99457 and 99458 require documentation of time spent monitoring and engaging with patients, including: • Total minutes of service per month. • Dates and brief notes on patient contacts. • Notes on data evaluation, trends, and related decisions. |
| Care Coordination and Patient Communication | All communication and coordination based on RPM data must be documented, including: • Secure messages, phone calls, and video visits. • Changes to care plans based on RPM. • Interactions with caregivers or family. |
| Adherence to HIPAA Standards | Documentation must meet HIPAA standards for data privacy and security, including the following checklist: • Data is encrypted. • Secure login/authentication protocols. • Patient consent for electronic communication is obtained. |
| Generate Monthly Summary Reports | A monthly report should summarize RPM activity and maintain an audit trail, including: • Number of days monitored. • Vital sign trend summaries. • Clinical actions taken. • CPT codes used for billing. |
| Tools and Platforms to Streamline Documentation | Platforms like HealthArc help automate and streamline documentation and provide benefits, including: • Auto time-stamp of data transmissions. • Automatic tracking of clinician time. • EHR integration. • Billable documentation from the start. |
Insurance Coverage for Remote Patient Monitoring (RPM)
| Section | Details |
|---|---|
| 1. Medicare Reimbursement for RPM | Medicare is a leader in encouraging RPM services, especially with the recent expansion of telehealth during the COVID-19 Public Health Emergency.
Key Takeaways: Medicare typically reimburses 80% of the approved cost, and the patient is responsible for 20%, unless they have a supplemental insurance plan. |
| 2. Medicaid Coverage Varies by State | Medicaid coverage is up to the authority of each state. Many states followed Medicare’s lead, but each has created individualized guidelines. For example:
• California: Covers RPM for management of chronic conditions with certain requirements. Providers need to check their state’s Medicaid manual or contact the state Medicaid agency for specifics. |
| 3. Private Insurance Coverage | Most private payers provide some form of coverage for RPM, especially in value-based contracting and employer-sponsored arrangements. Common coverage includes:
• Remote monitoring for chronic disease management (e.g., diabetes, hypertension) Some of the key insurers providing RPM services include UnitedHealthcare, Blue Cross Blue Shield, Cigna, and Aetna. Every payer’s plan is different, so it is always best to check with the insurance provider. |
| 4. Veterans Affairs (VA) Approaches to RPM | The VA is leading the charge in using RPM to manage chronic conditions in veterans via VA RPM Programs that provide:
• Free devices and data plans for veterans |
| 5. Coverage Levels and Restrictions | Regardless of the payer, RPM services must meet specific coverage criteria to qualify for reimbursement.
Common Requirements: Common Limitations: |
| 6. Device Coverage | The cost of RPM devices may be reimbursed by insurers in several ways:
• Rental – Devices can be rented to patients The device cost is typically included under CPT code 99454, which relates to the supply and transmission of the device. |
| 7. Co-pays and Out-of-Pocket Costs | Patients, even if covered by insurance, may incur co-pays, deductibles, and other out-of-pocket costs, including:
• Medicare: 20% coinsurance unless covered by a Medigap plan |
| 8. Value-Based Care Models | RPM is frequently a part of value-based care contracts, where providers are compensated for quality outcomes. Some examples include:
• Reduced ER visits and hospital readmissions Value-based care models often encourage payers to invest in RPM as a cost-saving and quality improvement measure. |
| 9. Emerging Coverage Trends for 2025 | Recent changes indicate a movement toward broader RPM insurance coverage. Some trends include:
• Increased support for mental health & behavior monitoring The CMS Innovation Center is also testing new models to promote RPM use in primary care and underserved populations. |
| 10. Confirming Successful Reimbursement | Healthcare providers can confirm RPM reimbursement eligibility if they:
• Verify insurance eligibility and coverage before enrollment |
With reimbursement for Remote Patient Monitoring expanding rapidly, there is support from Medicare, Medicaid, private insurers, and the VA, each providing varying levels of reimbursement to facilities and providers, and increasing support for patients. Insurance coverage for RPM is evolving daily, and its inclusion as part of standard care delivery is undeniable.
Providers and patients must understand what is acceptable, reimbursable, and allowable under RPM guidelines. Value-based care and other innovations are driving investment, permanent billing models, and operational support. RPM is poised to become a core part of modern reimbursable health services.
Remote Patient Monitoring (RPM) Billing Guidelines – 2025 Edition
- Overview of RPM Billing
RPM billing follows the Medicare Physician Fee Schedule (MPFS) structure, and there are multiple Current Procedural Terminology (CPT) codes that dictate how and when these services can be billed, including device setup, patient monitoring, and time spent on data analysis. Private payers and Medicaid plans have been aligning their reimbursement structures with CMS policies.
- Important Billing Guidelines
To bill for RPM, it must be established that:
The patient has a chronic or acute condition that requires monitoring.
The RPM device is FDA-cleared/approved and allows for automatic data upload.
Data was collected for 16 or more days within a rolling 30-day billing window.
The services were referred by a physician or qualified healthcare provider.
The patient’s consent to monitor their data, and that it was clinically relevant, must be documented.
- CPT Codes for RPM Billing
| CPT Code | Service Description |
|---|---|
| 99453 | Device setup and patient education |
| 99454 | Device supply and daily recording per patient |
| 99457 | First 20 minutes of interactive communication |
| 99458 | Additional 20-minute increments |
| 99091 | Collection and interpretation of physiologic data |
- Standards of Compliance and Documentation
Providers must include the following in clinical documentation:
Start and end date of monitoring
Data trends, if clinically relevant
Patient communications
Completed patient consent forms and a signed physician order
- Best Practices for Billing
Confirm payer-specific rules, as Medicaid and commercial payers often differ from CMS.
Use RPM platforms that integrate with patients’ EMRs to streamline documentation.
Conduct periodic training for clinical and billing staff.
Perform mock audits to check the accuracy of clinical documentation.
- Challenges to Reimbursement
Audited claims due to incomplete documentation
Use of devices not cleared by the FDA
Misalignment between billing and data collection periods
Inadequate documentation for interactive communication codes
- RPM Billing in Value-Based Care
The increase in value-based care models makes RPM billing worthwhile. Reduced hospitalizations, improved medication adherence, and better chronic disease management are all desired outcomes that align with value-based goals. Many ACOs and health systems have adopted RPM as a key component of their population health strategy.
- What Will Happen in 2025?
Increase oversight and scrutiny to identify and reduce RPM fraud
Add conditions eligible for reimbursement under RPM
Shorten the required streak of 16 collected days for certain high-risk patients
Clarify RPM policy in the behavioral health space
- What Are Some Billing “Don’ts”?
Don’t forget to amend payer contracts for RPM services.
Don’t use outdated CPT codes.
Don’t forget to obtain patient consent.
Don’t forget to track time associated with CPT codes 99457/99458.
- CMS Reimbursement Trends (2024–2025)
Approximate national average rates (non-facility settings):
| CPT Code | Avg. Rate (2025) |
|---|---|
| 99453 | $19.38 |
| 99454 | $55.77 |
| 99457 | $50.18 |
| 99458 | $40.84 |
| 99091 | $60–$72 |
- Cost Breakdown of RPM Programs
Device Costs: $25–$150/unit or $15–$30/month (leasing)
Software Costs: ~$10–$30 per patient/month (PPPM)
Personnel Costs: 30–60 minutes per patient/month
- Provider ROI Considerations
If done well, an RPM program can provide ROI within 3–6 months. A practice with 100+ eligible patients may earn $20,000–$30,000/month in new revenue, depending on staff and software efficiencies.
- RPM Reimbursement – Medicaid & Commercial
Commercial Payers:
– Aetna, Humana, and BCBS align with CMS policies.
– UnitedHealthcare uses hybrid RPM + virtual models.
Medicaid Reimbursement (as of 2025):
35+ states reimburse for RPM
Strongest coverage: Texas, California, New York, Colorado
Some require prior authorization or condition-specific eligibility
- Patient Costs
Medicare patients are responsible for a 20% coinsurance after the deductible unless they have Medigap or supplemental insurance. Commercial plans may require cost-sharing unless waived.
- Common Reimbursement Challenges with RPM
Variable private payer coverage
Denials from lack of documentation
Staff not familiar with specific billing nuances
- Solutions to Improve RPM Reimbursement
Bundle RPM with CCM or BHI services
Use daily time-tracking tools for billing (99457/99458)
Conduct regular audits of your documentation and coding
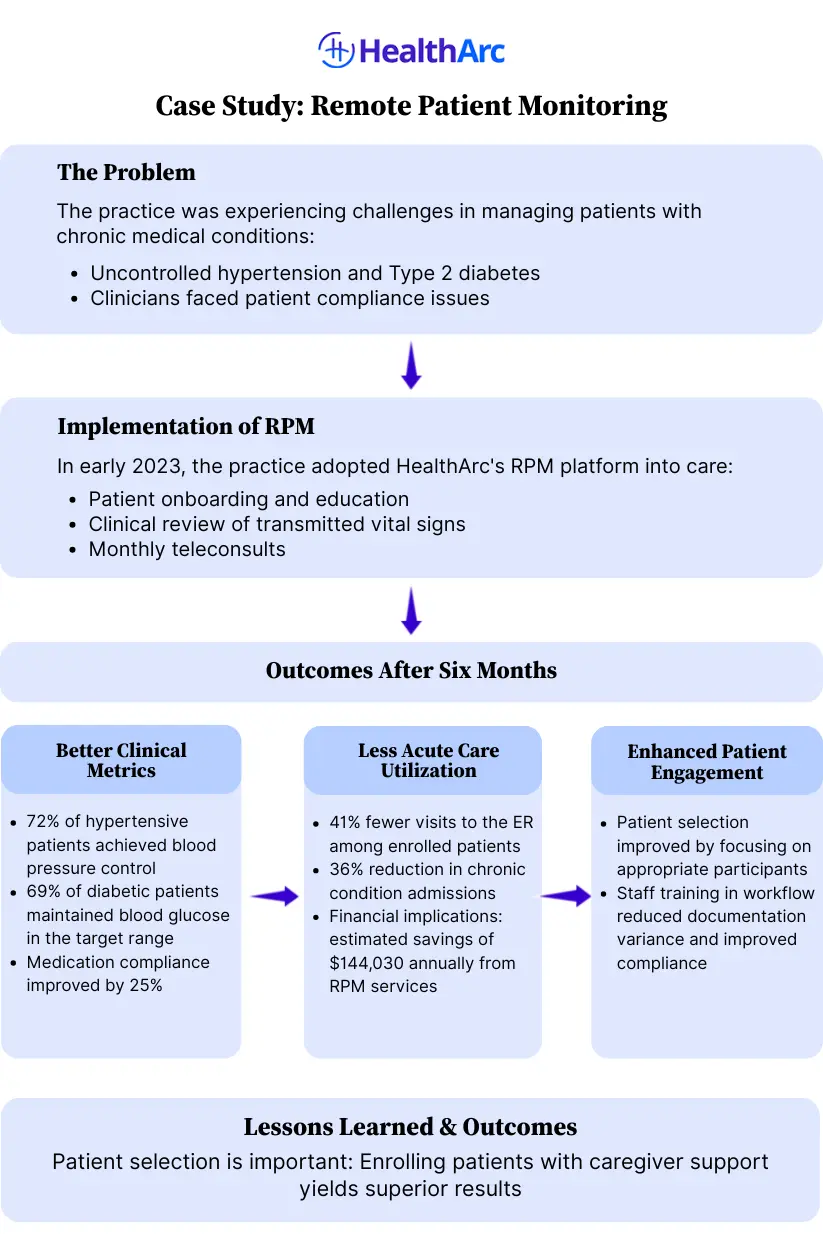
Case Study
Future Trends: What Lies Ahead for RPM Software & Devices?
Advancements in technology are expanding RPM capabilities beyond simple data capture and movement towards real-time analytics, predictive care, and personalized engagement. Here are some key trends shaping the future of RPM:
- AI-Powered Devices for Predictive Analytics: Next generation RPM devices will utilize AI to convert raw health data into actionable insights. These systems will be able to recognize early signs of deterioration, assess risk scores, and notify clinicians of potential issues before symptomatology worsens. For example, AI algorithms could look at heart rate variability and predict a potential cardiac event or trends in glucose levels that indicate an impending hypo- or hyperglycemia with high probability.
- Smart Inhalers to Manage Asthma and COPD: Smart inhalers with sensors across the inhaler track the medication use, inhaler technique, and frequency of rescue inhaler use. The inhalers transmit real-time data to care teams, and alerts can be sent should the patients’ patterns of use indicate the patient is non-compliant or experiencing poor disease control. Smart inhalers are particularly useful for chronic respiratory diseases, like asthma and chronic obstructive pulmonary disease (COPD), to manage patient’s adherence and reduce hospitalization.
- Lightweight Patch Monitors to Support Continuous Biometric Monitoring: Modern patch-based wearables, which require no vests or batteries, can replace heavier Holter monitors. Patch monitors can offer 24 hours of continuous ECG, respiratory rate, skin temperature, and motion tracking but without the heavier apparatus. Ultimately, the goal of using patches is to monitor patients for longer duration (days/weeks), as opposed to a traditional ambulatory diagnostic approach which is partial, and finally, to improve adherence from the patient standpoint by improving comfort/interface.
- Voice-enabled RPM Devices: For older adults, visually impaired, or trail limited mobility patients, getting advice through voice-enabled RPM tools are much easier for those patients to interact with RPM platforms. Patients can use natural language and engage with the RPM platform, ask health-related questions, report symptoms (when more than a yes or no response is wanted), and dispense medication reminders without having to drill down through complex good for touchscreens or cellular app interfaces.
- FDA-Approved Wearables with Clinical Use: Leading consumer products such as the Apple Watch, Fitbit Sense, and Samsung Galaxy Watch received FDA clearance as having clinical capacity to use features such as, but not limited to, an electrocardiogram (ECG), atrial fibrillation (AFib) detection, and blood oxygen (SpO₂) features. Consumer wearables represent a new avenue for patients to access remote monitoring by leveraging devices they already own and use in their daily lives, as opposed to lifestyle wearables, providing a continuum of consumer and clinical-grade RPM.
- Behavioral Biomarkers in Mental Health Monitoring: RPM’s expansion into mental health is an extension of the how facial expression, sleep, calendar, and smartphone usage behaviors are analyzed. AI-model-driven platforms can recognize and detect early warning signs of symptoms associated with depression, anxiety, or being bi-polar. This type of behavioral biometrics creates a low-touch way to monitor mental wellness, and enable early interventions in a pre-symptomatic state.
Remote Patient Monitoring (RPM) Services by HealthArc
HealthArc is a leading digital health platform specializing in Remote Patient Monitoring (RPM), Chronic Care Management (CCM), and Remote Therapeutic Monitoring (RTM) services. HealthArc has developed a comprehensive approach to implement RPM programs so that healthcare providers can positively impact clinical outcomes without increasing their resources and administrative burdens. Some of the key functionalities offered by an RPM platform include:
- Real-time patient monitoring: HealthArc’s RPM platform directly works with and automatically collects vital health data from patients via devices, such as blood pressure, weight, blood glucose, oxygen saturation, and ECG.
- Automated alerts: The HealthArc AI dashboard tracks abnormal trends and alerts our care teams automatically.
- EHR integration: Bi-directional interoperability with leading EHR vendors (Epic, Cerner, Athenahealth) to support documented coordinated care.
- Patient mobile applications: HealthArc provides patients with mobile apps to ensure continued engagement through alerts, reminders, daily logs, and health tips.
- Patient-centered care plans: HealthArc allows providers to customize treatment protocols for care plans based on conditions, such as diabetes, hypertension, CHF, and COPD.
- FDA-approved devices: HealthArc provides a catalog of FDA-approved remote monitoring devices upon shipping to patients, including:
• Bluetooth blood pressure cuffs
• Cellular-enabled weight scales
• Smart glucometers
• Pulse oximeters
• ECG patches and heart monitor patches
All devices are plug-and-play (easy-to-set-up) for patients. Devices are HIPAA-compliant and FDA-compliant in terms of online security.
- Provider and Patient Support
• Patient engagement: Multilingual support, device onboarding, training.
• Clinical monitoring: 24-hour clinical teams available to intervene when necessary.
• Billing compliance: Aids providers in navigating and maximizing RPM reimbursement; coding and claim submission are included.
- Results and Outcomes
Clients that have been using the HealthArc platform report:
• Hospital readmissions reduced by as much as 50%
• Patient adherence improved by 70% within three months
• Care teams are more efficient
• Uplift in revenue for exploring proper and available billing codes (CPT 99453, 99454, 99457, and 99458)
HealthArc is more than a technology vendor; we are a digital healthcare partner working to improve patient outcomes, reduce clinician burnout, and change the healthcare delivery model through scalable and reliable RPM solutions.
Enhance Patient Outcomes With HealthArc’s RPM Platform
Remote Patient Monitoring has become a present and future reality of proactive, just-in-time care. The many benefits that RPM offers include, improved outcomes, decreased costs, sustainable ongoing patient engagement, and empowerment of providers and patients, making it an integral part of modern day healthcare models.
The urgency of value-based healthcare, the emphasis on chronic disease management, and demand for convenient monitoring solutions have made RPM delivery models one of the best choices for delivering personalized care to chronic patients.
RPM is an integral part of the healthcare delivery model, especially for those in the aging population, rural communities, and individuals with chronic conditions. It allows for improved clinical efficiency, broader access to patient data, increased patient engagement, and reduced unplanned hospitalizations. Patients benefit from the convenience of scheduling, ongoing monitoring, early recognition of deterioration, and lessened isolation from their care teams.
HealthArc has truly accelerated to the forefront by providing HIPAA-compliant RPM solutions for small clinics, solo practices and large health systems. Its end-to-end remote monitoring platform with real-time analytics, device integrations, and automated workflows makes remote care easy, while keeping the reimbursements high for providers.
If you are a healthcare organization, physician, or health tech innovator looking to implement RPM or improve your existing digital health capabilities, now is the time. Keep yourself informed, connected, and engaged in the remote care industry with the latest RPM software. Request a free demo now to learn how HealthArc integrates RPM, CCM, and AI to reduce hospital readmissions and improve health outcomes.
Frequently Asked Questions (FAQs)
As of 2025, CMS reimburses RPM services for the following CPT codes:
- 99453 – Setup of device and educate patient, one time: $19.73
- 99454 – Device supply and data transmission, for the month (16+ days):$43.02
- 99457 – First 20 minutes of RPM treatment management: $47.87/month
- 99458 – Each additional 20 minutes: $38.49
These rates promote the convenience of chronic and acute care monitoring when using FDA-approved, connected devices.
- RPM is used as recorded physiological data (i.e., blood pressure, glucose) through FDA-approved, connected devices, and for a minimum of 16 days a month;
- CCM is used with patients with two or more chronic conditions to emphasize care coordination and medication management through ongoing communication, not device data.
- RTM uses a software application or similar application, and data will reflect adherence to therapy and musculoskeletal status, and is typically used in Physical or Respiratory Therapy. Unlike RPM, the patient self-reports the data for RTM.
Medicare and many Medicaid Plans pay for RPM:
- Patients with chronic or acute collections requiring monitoring;
- FDA-approved devices, used in connection with the automatic transmission of information;
- data tracked for a minimum of 16 days in 30 days; and,
NOTE: State regulations on Medicaid change; therefore, providers have to check state rules.
Devices and platforms used for RPM must comply with HIPAA requirements as follows:
- Encrypted during transmission end-to-end
- Encrypted data storage that is stored encrypted (storage encryption)
- Use of access controls, audit logs, and role-based permissions to protect patient information
- RPM vendors generally use cloud-based, HIPAA-compliant platforms that secure patient privacy and security at all relevant points.
Yes, contemporary RPM platforms leverage artificial intelligence and predictive analytics to identify early signs of clinical deterioration by analyzing trends within vital signs and physiologic data. These trends enable providers to initiate a proactive intervention prior to the patient visiting an emergency room.
Platforms used for RPM will incorporate interoperability standards including (but not limited to) Fast Healthcare Interoperability Resources (FHIR), HL7 and RESTful APIs to ensure seamless integration into EHR systems as it relates to data exchange and coordination of care.
RPM provides the opportunity to circumvent access barriers to healthcare by providing remote monitoring, thus alleviating travel concerns, encumbering continuity of care and access to healthcare, especially for patients in rural settings and geographically underserved areas, thereby closing the access gap to improve health equity and outcomes.
Providers intending to bill CTP 99457 must document:
- Patient consent (verbal or written)
- Person providing real-time interaction (≥20 minutes/month by clinical staff or provider)
- Treatment management decisions involving the RPM data
- Date, duration, and content of the service
To receive reimbursement from Medicare for CPT 99454, RPM data must be collected and transmitted for 16 days or more in 30 days using an FDA-designated connected device.
Key barriers to RPM are lack of digital literacy, lack of broadband access, difficulty integrating RPM into workflow, and provider buy-in. To overcome barriers, patients need RPM education, easy-to-use devices, integration with the EMR, and staff training in RPM protocols.
RPM programs have a huge effect on reducing hospitalization and readmissions associated with chronic conditions such as heart failure, COPD, and diabetes, through early detection and intervention, as well as enhanced patient compliance.
Most Recent Blogs
Categories
Related Blog
- February 13, 2026 | Read Time: 8 mins
CPT 99445 and 99470: Complete 2026 Guide to Short-Window RPM Billing with HealthArc
CPT 99445 and CPT 99470 are transforming how practices bill for Remote...
Learn More- January 24, 2026 | Read Time: 15 mins
Care Gaps in Healthcare: What They Mean, and How to Close Them Faster
There has always been a lot of data in healthcare. The challenge...
Learn More- January 8, 2026 | Read Time: 11 mins
Top 5 Vitals That Drive Better Outcomes in Remote Patient Monitoring Programs
As per various studies and well documented reports on managing chronic illnesses...
Learn More


