How Remote Monitoring & AI Are Tackling Burnouts in Small Practices?

Approximately half of U.S. physicians experience symptoms of burnout, including exhaustion, cynicism, and reduced work effectiveness. Your small practice should not be troubled by staffing shortages and clinician burnout.
Remote Patient Monitoring (RPM) and Artificial Intelligence (AI) can offer a solution to this ever-rising issue. By amplifying the efforts of a limited staff and automating time-consuming tasks, they can help reduce the burden and prevent burnout among physicians and their staff.
Discover how technology can alleviate the burden and mitigate such issues in this comprehensive guide.
Table of Contents
ToggleWhy are small practices struggling with staffing and burnout?
Small private practices are feeling the squeeze, and rising patient demand, combined with limited hiring budgets, is the reason. By 2034, the U.S. could be short up to 124,000 physicians.
Nearly 45% of doctors report at least one symptom of burnout, and most of them come from small practices. These issues are further intensified and must be proactively addressed
Remote Patient Monitoring: The secret weapon to do more with less
Remote Patient Monitoring is an impactful tool that allows patient monitoring without leaving the clinic. It reduces the overall burden on doctors, leading to fewer cases of burnout. With this strategic investment, a small practice doesn’t require amplified budgets for hiring. Here’s how RPM can help-
- Reduced in-person visits for patient checkups- Routine checkup, including analysis of patient’s vitals, can be done remotely with the help of RPM. This frees up appointment slots and staff’s workload. Staff or doctors require in-person visits only in case of an intervention or special concerns.
- Avoided crisis due to early detection of patient issues- Burnout often sets in during or after managing a crisis. Remote Patient Monitoring (RPM) helps identify early warning signs, allowing for timely intervention and preventing the situation from escalating into an emergency.Avoiding emergencies and a proactive and controlled workflow leads to less stress and burnout.
- Centralized Monitoring—RPM empowers one nurse to monitor dozens or more patients with a glance on the dashboard. With the help of RPM, the centralized remote monitoring team at Veterans Health Administration witnessed a 33% decrease in hospital admissions. To accomplish this, one employee was dedicated to monitoring RPM systems, and the overall burden of others was reduced, leading to higher efficiency.
- Encourages patients to self-manage their health- RPM is a powerful tool that prompts patients to take more responsibility for their health. Patients are more engaged and adherent, leading to better results of treatment and a healthier body.
Here is a table illustrating the difference RPM makes on workload impact.
| Challenge | Traditional Approach | Remote Patient Monitoring |
|---|---|---|
| Tracking patient vitals | Frequent in-person visits or calls consuming more time | Patients measure vitals at home, directly sending the data to the clinics. |
| Managing risks in chronic patients | Symptoms are discovered late, leading to emergency intervention. | Alerts notify staff of concerns regarding trends leading to a controlled situation. |
| Number of routine follow-ups | Regular one-on-one follow-ups (visits and calls) leading to an increase in the patients per staff ratio. | One nurse can monitor several patients at once via a remote dashboard. |
| Patient engagement and adherence | Patients wait for doctors and often lack initiative-taking care. | Patients are motivated through self-monitoring, take readings consistently. This reduces the burden on clinics and staff. |
AI Tools- Free your staff from administrative overload
AI tools can reduce the administrative workload that leads to burnout among the staff. Artificial intelligence in healthcare is mostly about using software and automating tasks that eat up staff’s time, so that they can focus on compassionate care. Here are the key areas where AI-driven tools help reduce the burden.
- Documentation– AI plays a crucial role in reducing the workload of staff by taking up the documentation process. Clinical intelligence systems can record conversations, listen to the doctors and the patients, and create a draft clinical note or summary. This is especially beneficial in capturing patient history, doctor’s assessment, diagnosis, and rules to follow. A recent study by JAMA Network Open found that using an AI assistant for documentation helped physicians reduce the time spent on EHRs by 30% and after-hours charting by 30%.
- Inbox management- AI automates replies to the flood of patient messages, prescription refill requests, and test results in the EHR box or patient portal. AI handles common patient inquiries, improving response time and care efficiency, , significantly reducing burnout and workload in clinicians. In other things, AI can send automated reminders to patients about appointments or lab follow-ups to reduce staff time spent on calling.
- Scheduling and billing- The staff at a small practice often juggles between several tasks, such as scheduling appointments, billing, verifying insurance, etc. Software with AI capabilities can handle these tasks, ensure efficiency while reducing workload. Tools like AI-based scheduling tools, coding assistants, and billing software can free up hours of staff time.
- Clinical insights- Using AI to reduce cognitive load is a smart move that can help small practices enhance operations. AI systems can integrate with remote monitoring platforms to offer exceptional clinical insights about their health. By pulling out key metrics and concerning factors from a patient’s reports, they can lessen the doctor’s burden. This helps reduce the risk of doctors becoming overwhelmed by data, ultimately lowering the likelihood of burnout.
Small practices that use AI for routine work save several hours each week, offering more time to patient care. Do not mistake this as removing the human touch from the loop. Consider this a partnership between humans and artificial intelligence to boost productivity and efficiency.
Adopting AI in a small practice isn’t expensive or difficult, given you partner with the right expert. Technology has devised affordable standalone services and comprehensive EHR services.
The first step is to identify the core issue that is leading to staff burnout, and then select the appropriate service to manage it. Over 65% of physicians who use an AI documentation assistant recommend it. The world is witnessing major workflow improvements by embedding the use of AI in its routine tasks.
Why is RPM+AI a game changer for small practices?
Remote Patient Monitoring expands clinical capacity by automating patient monitoring.
Here’s an example- The staff of a small clinic monitors patients via smart alerts, and AI manages the notetaking and inbox replies. The workload is shared efficiently, allowing your team to operate seamlessly Here’s why a combination of RPM and AI can be extremely beneficial for small practices.
- RPM extends clinical capacity.
- AI lightens the administrative load.
- A blend of both creates a sustainable workflow.
Let us help you understand with a use case.
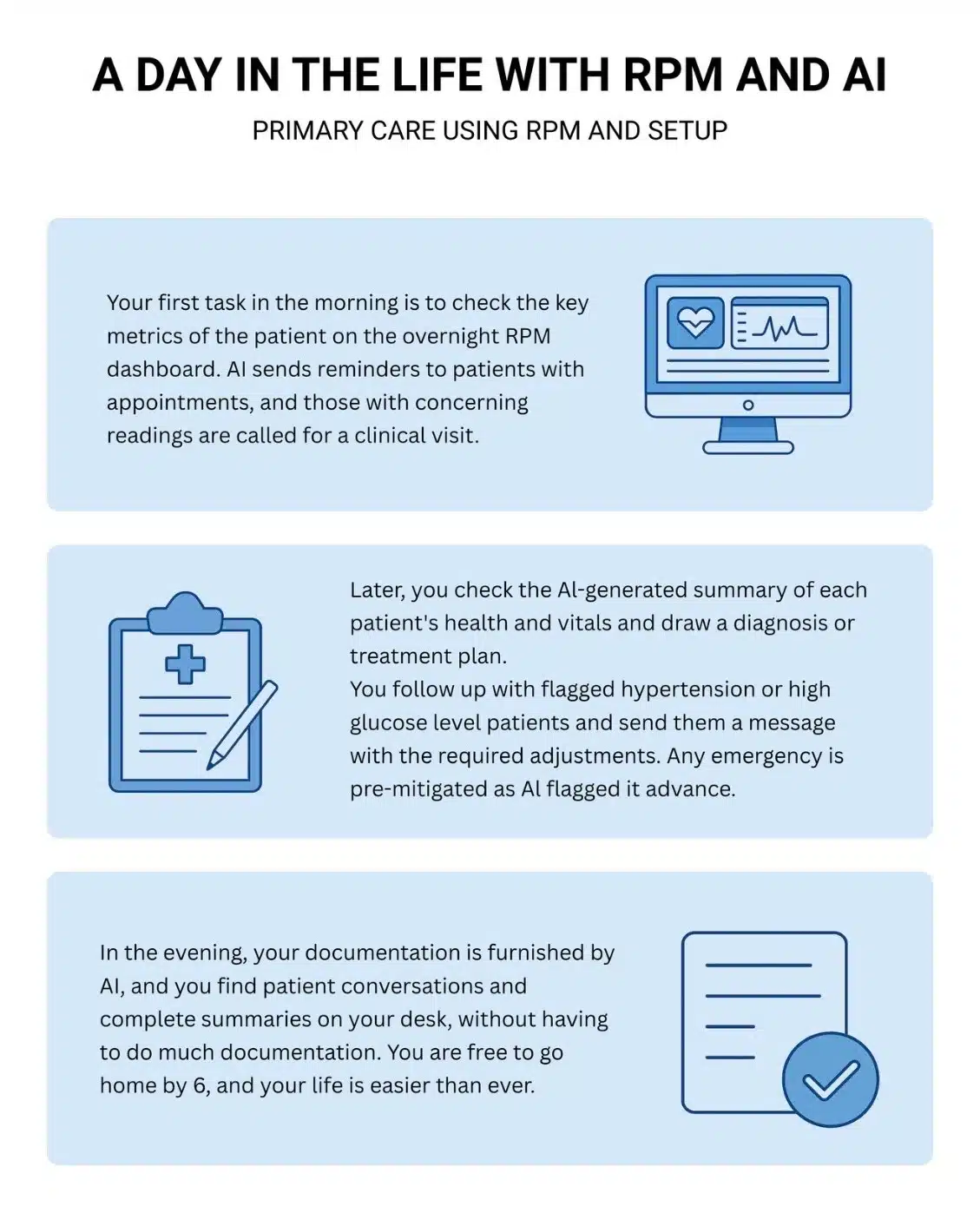
This scenario represents what your daily routine can be like a physician running a small practice. A combination of AI and RPM can reduce workload while also helping you financially. With improved billing accuracy and more patients addressed in a day (given the free time), your small practice can benefit exponentially.
You can offer continuous and comprehensive care, keeping patients healthy and happy without causing burnout amongst your employees. However, the implementation of RPM and AI must be carefully conducted. You can begin with RPM, reap its benefits, and slowly integrate AI into the plan.
Future Prospects and Government Initiatives
The US Government is offering exceptional support to small providers, including Medicare reimbursement policies and investments in public health informatics. This adds up to the promising prospects of Remote Patient Monitoring. The future of RPM includes broader integration into healthcare, aiming for better care for the patients and a lesser burden on the providers. This will result in improved patient outcomes and better treatments and results, especially for chronic diseases.
The near future will also witness increased integration of artificial learning (AI) for efficient data analysis and personalized care. In the US, several funds, such as the Distance Learning & Telemedicine Grants, prompts small practices to inculcate AI and RPM into their systems. Additionally, several government incentives encourage investment and the application of RPM devices to improve accessibility among patients.
Ready to lighten the load? Start small, scale smart!
Collaborate with Remote Patient Monitoring (RPM) and Artificial Intelligence (AI) to ensure that your small practice not only survives but also thrives. Start with one tool, such as RPM, and witness the impact on your workflow and stress levels. Grow from there to turn your small practice into an automated and smoothly operating setup.
Final Thoughts
While the staffing challenges prevail, introducing the combo of RPM and AI to your small practice can make all the difference. These tools help your staff focus on delivering compassionate care without burnout. For care providers, innovation is extremely important to improve outcomes for staff and patients.
Technology can never replace the compassion and expertise of human healthcare providers. However, it can ease their burden and improve results. As a healthcare provider, investing in tools that support your staff is an investment you must be ready to make.
By leveraging remote patient monitoring (RPM) and artificial intelligence (AI), you can thrive, deliver better care, and improve your staff’s quality of life and career.
Suggested Next Steps
Pick a common bottleneck you experience in your practice. Pilot a simple solution and witness the results. Start with a consultation with experts. Reach out to a trusted digital provider, such as Healtharc, that can help you build confidence with complete knowledge.
HealthArc uses AI-powered transcription to process accurate, real-time documentation of patient interactions. With advanced predictive analytics, data-driven decision-making empowers physicians to take proactive, outcome-focused interventions that improve patient care HealthArc’s AI capabilities streamline remote care management, promoting a high-quality care experience for patients and a seamless workflow for providers. Talk to HealthArc’s expert to learn more.
Frequently Asked Questions (FAQs)
No, technology works to assist your staff, not replace them. With RPM and AI, you can automate repetitive tasks and oversee more patients safely. Humans are still required for clinical judgment and personal interaction to promote quality care.
RPM and AI solutions are created as plug-and-play to offer utmost ease and comfort to small clinics. For the best results, you can partner with a provider that supplies ready-to-use devices with a simple dashboard and all the features you need. However, it’s recommended to start with one tool, become comfortable using it, and then gradually adopt others
Patients need extra attention, and tools like RPM can act as care providers, monitoring them every day. Remote monitoring can make patients feel more connected to the provider and more enthusiastic about their health and wellness. Tracking vitals regularly will keep them engaged and motivated to adhere to the treatment plan. With the help of a human touch, patients can be guided about the uses and benefits of integrating these devices into the plan. Those who are skeptical can be taught the use of RPM and AI tools in providing better care and greater results.
In this scenario, choosing a robust RPM and AI setup is quintessential. Privacy and security are critical considerations for all. Reputable solutions are accompanied by data protection via HIPAA-compliant encryption and other safeguards. Healthcare providers must make privacy a top priority and ensure consent before recording and using patient data. With proper implementation, RPM and AI do not expose patients to privacy risks.
The results of implementing RPM and AI in your practice are positive. These can be highlighted in terms of better patient outcomes, fewer urgent calls, less time for documentation and other administrative tasks, and additional revenue. Over time, you’ll see increased patient engagement, improved quality of care, stronger financial performance, and a happier, burnout-free staff. Integrating technology into your care model makes it more sustainable—and far more rewarding
Bibliography
- AAMC. (n.d.). AAMC report reinforces mounting physician shortage. Association of American Medical Colleges.
- American Medical Association. (n.d.). What is physician burnout?
- Jain, S., Misra, D. P., Rajadhyaksha, P., Negi, V. S., & Gupta, L. (2020). Telemedicine for rheumatology care in India: Projections during COVID-19 pandemic. Journal of Family Medicine and Primary Care, 9(11), 5607–5612.
- News VA. (2023, October 3). RPM, HT saves Veteran lives, reduces admissions. U.S. Department of Veterans Affairs.
- Telehealth.HHS.gov. (n.d.). Telehealth and remote patient monitoring: Billing for remote patient monitoring.
- U.S. Department of Agriculture. (n.d.). Distance learning & telemedicine grants. Rural Development.
Most Recent Blogs
Categories
Related Blog
- January 14, 2026 | Read Time: 12 mins
What Is a Care Manager? Roles and Responsibilities
A care manager is a dedicated healthcare professional who helps patients navigate...
Learn More- December 17, 2025 | Read Time: 9 mins
The ACCESS Model and the Platform Practitioners Need to Do Well in Outcome-Based Care
The change from volume-based healthcare to outcome-based care is no longer on...
Learn More- June 21, 2025 | Read Time: 8 mins
Chronic Care Management Trends 2025: CMS Updates, AI Tools & RPM Integration
While healthcare delivery has become more accessible, chronic conditions continue to impact...
Learn More


