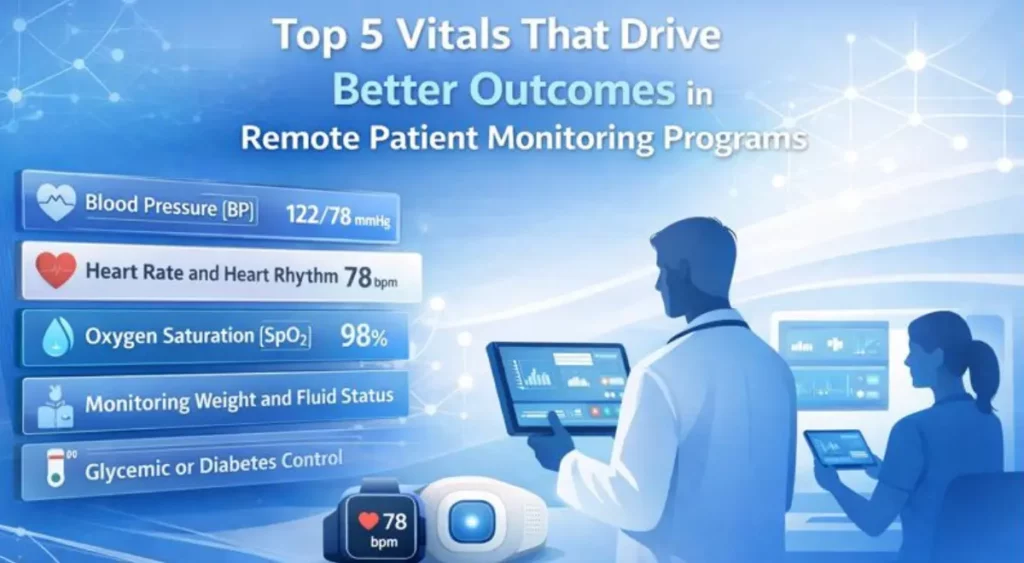
Top 5 Vitals That Drive Better Outcomes in Remote Patient Monitoring Programs
As per various studies and well documented reports on managing chronic illnesses among patients, Remote Patient Monitoring (RPM) delivered outstanding outcomes and is highly effective in chronic condition management and reduces avoidable hospital visits or emergency hospitalizations. RPM programs utilizing high-impact vitals reported helped in a reduction of up to 45% in hospital readmissions, a 30% reduction in emergency department visits, and a 20–35% improvement in chronic disease control metrics when implemented within 12 months of disease progression.
The drivers of these RPM outcomes are rapid clinical response times, ongoing visibility of patient data, and coordinated care that a contemporary RPM platform like HealthArc provides.
With the continued transition of healthcare systems to value-based care models, it is essential to understand which vitals truly affect outcomes so healthcare systems may develop scalable, clinically viable RPM solutions for chronically ill patients.
Table of Contents
ToggleWhy it is Important to Choose the Correct Vitals for a Successful RPM Program?
All vitals do not provide equal predictive or preventive management capability. In successful RPM systems, the selected vitals will indicate early signs of patient deterioration, provide direction to providers on how to best manage patient care, and align with the Centers for Medicare & Medicaid Services (CMS) reimbursement policy and billing guidelines.
Rather than monitoring a multitude of distinct data elements without a clinical pathway and without specific alert thresholds, successful RPM creates an environment where the clinical staff makes focused, evidence-informed choices within a single, comprehensive view of patient vitals, with the inclusion of automated escalation workflow processes and patient engagement tools.
Blood Pressure (BP)
Blood pressure is one of the most vital measures for monitoring patients’ health in the remote monitoring services sector, making it one of the most widely used vitals. Half of adults in the United States have been diagnosed with hypertension which remains mostly uncontrolled due to limited opportunity for monitoring by healthcare providers.
Continuous or routine monitoring helps providers detect trends in blood pressure, identify early intervention options, and ultimately prevent the development of serious complications like stroke, myocardial infarction, and kidney disease.
When patients are frequently diagnosed with high BP (hypertension) and do not experience any symptoms related to it, RPM provides an excellent way for healthcare providers to monitor their patients and identify risk factors that may lead to negative outcomes before the patient confronts an adverse event related to hypertension.
RPM for Blood Pressure Management: RPM for BP offers many benefits to patients who have hypertension, heart failure, chronic kidney disease, need post-stroke recovery, and are at high risk for pregnancy or postpartum complications.
By monitoring BP for patients at risk, clinicians can identify opportunities to adjust medications, provide telehealth visits, and provide education on healthy lifestyle choices. These interventions can ultimately reduce a patient’s need to be hospitalized for hypertension-related issues.
An effective RPM platform integrates FDA-cleared BP cuffs that automatically transmit data to the provider, longitudinal analysis of BP trends, and alerts for providers. The RPM platform eliminates the potential for errors associated with manual reporting and enables providers to have access to actionable insights as opposed to fragmented data.
Heart Rate and Heart Rhythm
Continuous and ongoing heart rate and rhythm monitoring are critical components of a systematic approach to the early detection of cardiovascular instability, before it becomes critical or life-threatening.
The detection of irregular or dysrhythmic heart rhythm abnormalities increases the risk of stroke, and is frequently not detected in traditional hospital settings.
RPM for Heart Rate Monitoring: Remote Patient Monitoring for cardiac patients allows for the real-time correlation of heart rate trends and reporting of related signs and symptoms, such as dizziness, fatigue, and palpitations.
Continuous or frequent monitoring significantly improves diagnostic accuracy and reduces the treatment complications, especially in older adults and high-risk cardiac patients.
Using RPM with wearable ECG patches, as well as smart devices and pulse oximeters provides clinicians with passive sources of heart rhythm data capture. By using advanced analytics to automatically detect rhythm abnormalities, notifications are sent to the clinical team, leading to earlier intervention and increased patient safety.
From the perspective of providers, RPM eliminates the need to conduct unnecessary visits to doctors’ office, facilitates early detection of AFib (Atrial Fibrillation), and supports proactive management of anticoagulation therapy, thereby providing both clinical and financial benefits.
Oxygen Saturation (SpO₂)
SpO₂ is an early indicator of respiratory and cardiac compromise. By monitoring SpO₂ remotely, clinicians may identify deterioration in a patient’s condition long before the patient demonstrates signs of distress.
A patient who experiences an abrupt drop in their SpO₂ may potentially indicate infection, an exacerbation of their pulmonary condition, or decompensation of their heart failure. Early identification of these conditions through the use of RPM will permit timely adjustment of medications, the initiation of supplemental oxygen, and/or potentially rapid escalation to in-person care.
RPM for SpO₂ Monitoring: Monitoring SpO₂ is critical for patients with COPD, asthma, post-surgical recovery needs, heart failure, and long COVID. RPM programs that incorporate respiratory monitoring consistently reduce hospitalizations and improve symptom management.
When integrated with an RPM services platform, pulse oximeters automatically send pulse oximetry readings directly to the remote monitoring platform and alert the provider when readings exceed a certain threshold. This allows clinicians to monitor the patient more effectively as they receive comprehensive views of their patient’s condition, in addition to an isolated view of the pulse oximetry reading.
Monitoring Weight and Fluid Status
The daily monitoring of weight is considered one of the most reliable indicators for the onset of worsening heart failure and/or fluid overload. Small increases in weight can indicate fluid retention up to several days before the onset of symptoms.
RPM for Weight Management: Monitoring weight remotely gives the clinician the opportunity to act sooner by adjusting diuretic therapy, providing dietary counseling, or scheduling a telehealth visit to prevent hospitalization. Monitoring weight enables clinicians to determine how well the patient’s medications are working and how adherent the patient is to their prescribed regimen.
Connected digital scales automatically send patients’ daily weight readings into the RPM system and alert the clinician if there is a significant trend. When paired with symptom reports such as swelling or shortness of breath, monitoring weight can offer an efficient way to identify patients who are approaching deterioration or the development of heart failure symptoms.
Remote Patient Monitoring programs with weight monitoring show lower rates of readmission and increase patient confidence in self-management within 30 days of discharge.
Glycemic or Diabetes Control
Effective glycemic control of diabetes is critical for optimal diabetes management, as diabetes is one of the most common and costly chronic diseases in the United States. Poor glycemic control can cause significant complications that adversely affect quality of life and increase healthcare costs.
RPM for Diabetes Control: The use of RPM to monitor blood glucose provides clinicians with a continuous or periodic stream of information to identify trends in blood glucose management. By being able to see real-time glucose fluctuations as well as medication changes, clinicians can proactively manage their patients’ care to limit the occurrence of hyperglycemia and hypoglycemia. It also allows patients to see how their diet, exercise, and medications are affecting their blood glucose level on a per-day basis.
Additionally, many modern RPM systems can integrate continuous glucose monitors (CGMs) as well as standard glucometers, allowing clinicians to see how their patients are managing their blood glucose over time to evaluate and address fluctuations in blood glucose levels. Alerts generated from the system help identify potentially risky blood glucose patterns such as nocturnal hypoglycemia, as well as prolonged hyperglycemia.
Over time, effective RPM for diabetes management can improve HbA1c readings, decrease complications, and support long-term population health and management goals.
How RPM Programs Ensure Effective Clinical Actions Via Vitals Monitoring?
While vitals alone are not enough to improve outcomes, taking action based on vitals helps improve outcomes. By utilizing structured workflow and care coordination, a high-performance RPM program is able to intervene in a timely manner with a patient.
Having clear escalation protocols on when a clinician should contact a patient, modify a patient’s medication, or schedule a visit increases overall safety and ensures that no escalated vital signs go unnoticed.
It is essential to engage, remind, educate the patient, and allow for secure messaging between the provider and patient tend to have more adherent patients, which yields better outcomes. When a patient is engaged, they will properly use the device and follow the care plan.
From a sustainability perspective, automated documentation workflow and coding workflow help support RPM billing as well as Chronic Care Management (CCM) reimbursement, reduce the administrative workload, and protect the long-term financial viability of the RPM program.
Best Practices in Developing a Successful RPM Program
A successful Remote Patient Monitoring (RPM) program is formulated keeping in mind the provider and patient goals, selecting the right patients and vitals, using FDA-approved devices, implementing a scalable RPM platform, engaging patients, and optimizing reimbursement workflows. Here’s a step-by-step guide to developing a RPM program.
Step 1: Define Goals
Clearly define the clinical and business goals for implementing Remote Patient Monitoring, as well as what the provider focuses on achieving through implementing this program (reducing readmissions, improving chronic disease management, and creating a value-based care strategy). These goals will then drive your technology, staffing needs, and workflow decisions.
Step 2: Identify the Right Patients
Providers need to focus on their efforts of monitoring high-risk patients who would benefit from continuous monitoring, such as those dealing with hypertension, heart failure, diabetes, or Chronic Obstructive Pulmonary Disease (COPD). Selecting the right patients will result in better outcomes and increased overall efficiency of your RPM program.
Step 3: Select Actionable Vital Signs
In order to have a successful RPM program; you will need to focus on actionable vital signs. These include blood pressure, heart rate & rhythm, oxygen saturation, weight, and blood glucose. Each of these VSS corresponds to a direct line of action or clinical intervention pathway.
Step 4: Use FDA-Cleared Devices and Scalable RPM Platforms
You will need to implement reliable, FDA-cleared RPM devices into your centralized RPM platform. Cellular wireless connectivity allows for greater ease of use and improved connectivity, which results in better adherence.
Step 5: Create Clinical Workflows and Escalation Procedures
Create alert thresholds, establish who will respond, and define the steps for escalation. Having a structured workflow ensures that abnormal data results in the timely delivery of patient care without burdening your staff.
Step 6: Build Patient Involvement and Knowledge
Onboarding, educating, and providing reminders are essential to a patient’s ability to stay compliant. When patients are engaged, the data they supply is more consistent, and they achieve better results.
Step 7: Streamline Billing and Performance Tracking
Automated documentation can support reimbursement for remote patient monitoring services and chronic care management activities, while performance tracking allows for ongoing monitoring of RPM programs over time.
Effective RPM programs lead to improved patient outcomes while reducing utilization and providing sustainable value to providers when they are effectively designed.
Some Frequently Asked Questions (FAQs) for Providers About RPM Programs
Blood Pressure, Heart Rate/Rhythm, Oxygen Saturation, Weight, and Blood Glucose are the top five with the greatest clinical and financial impact in remote patient monitoring.
Yes, RPM reduces provider workload by utilizing centralized RPM platforms equipped with smart alerts and automation.
Yes, RPM services and Chronic Care Management (CCM) are reimbursable under CMS CPT codes.
Patients with hypertension, heart failure, chronic obstructive pulmonary disease (COPD), diabetes, and post-acute care needs benefit most from RPM.
Utilization reduction, improved outcomes, and performance improvement on quality measures support value-based care.
Streamline Your RPM Program’s Success with HealthArc’s Digital Health Platform
The success of RPM services for healthcare providers is dependent upon monitoring vitals that are critical for clinical decision-making. A complete RPM program includes blood pressure, heart rate/rhythm, oxygen saturation, weight, and blood glucose. Coupled with a scalable RPM platform, these vitals positively ensure reducing readmissions, improving chronic disease management, and providing long-term financial viability.
HealthArc provides remote patient monitoring services to healthcare providers throughout the U.S., as well as an integrated RPM platform featuring the integration of FDA-approved devices, automated billing processes, connections between Electronic Health Record (EHR) systems, and care coordination tools.
Together, these features support the growth of RPM programs focusing on increased medical care, reduced costs, and success in value-based care. Need help implementing an RPM program? Feel free to schedule a demo or call us at +201 885 5571 now for more information on our monitoring programs, billing and eligibility.
Most Recent Blogs
Categories
Related Blog
- February 20, 2026 | Read Time: 12 mins
How Remote Patient Monitoring Helps in Mental Health Care Conditions
There is a structural change happening in mental health care. In recent...
Learn More- February 13, 2026 | Read Time: 8 mins
CPT 99445 and 99470: Complete 2026 Guide to Short-Window RPM Billing with HealthArc
CPT 99445 and CPT 99470 are transforming how practices bill for Remote...
Learn More- January 24, 2026 | Read Time: 15 mins
Care Gaps in Healthcare: What They Mean, and How to Close Them Faster
There has always been a lot of data in healthcare. The challenge...
Learn More


