Remote Patient Monitoring for Alzheimer’s
Alzheimer’s is a progressive neurological ailment that causes cognitive decline, memory loss, and behavioral abnormalities. Alzheimer’s disease affects around 6.9 million Americans aged 65 and older. By 2060, the number of impacted individuals is predicted to nearly triple to 14 million.
Early detection and monitoring of Alzheimer’s disease symptoms are critical for optimal care. Alzheimer’s disease presents with a variety of signs and symptoms, including memory loss, disorientation, changes in mood or behavior, and difficulties performing daily duties. The condition also presents substantial obstacles for patients and caretakers.
Table of Contents
ToggleImpact of Alzheimer’s Disease On Elderly Health
Alzheimer’s disease is more common in the elderly, although it can also affect young people. It is a progressive disorder that begins with mild memory loss and proceeds to loss of capacity to talk and respond to the surroundings. The disease’s symptoms may appear after the age of 60, and the risk rises with age.
Many Alzheimer’s patients are being cared for at home by family members. Although most people are eager to assist their family and friends, caring for someone with Alzheimer’s disease at home can be difficult and demanding at times. Every day, the caregiver adjusts to new abilities and behavioral patterns. People with Alzheimer’s disease usually require increasingly intensive care as the disease advances.
RPM Technology Solution for Alzheimer’s Disease
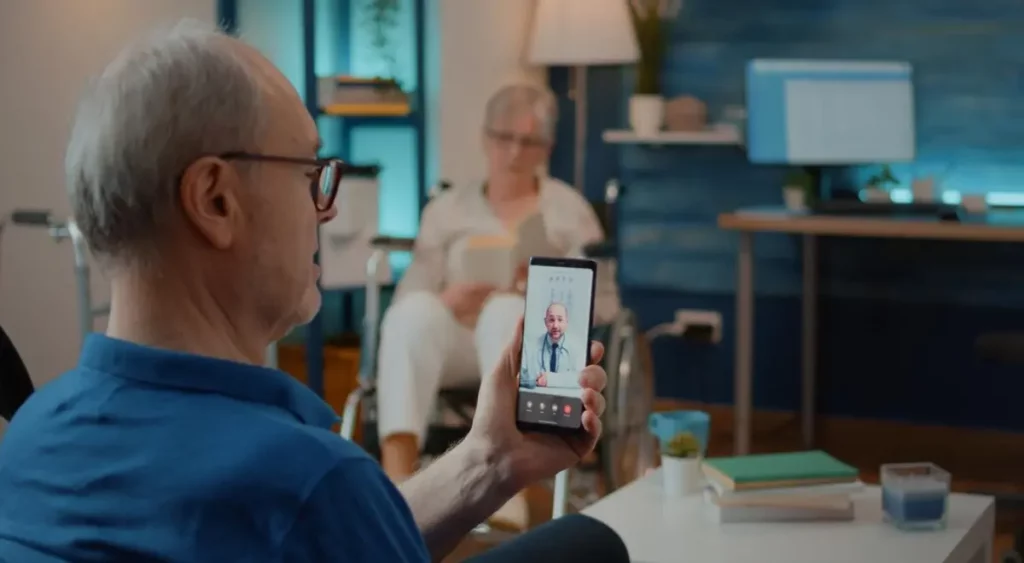
Remote Patient Monitoring (RPM) for Alzheimer’s disease can aid in determining cognitive and functional impairment in Alzheimer’s and dementia patients. RPM provides a realistic view of patients in their own homes.
Using modern technology, new and improved ways for accurately measuring functional decline in all phases of Alzheimer’s disease can be achieved through remote patient monitoring.
In this blog post, we will look at how RPM can be used to monitor Alzheimer’s disease care.
3 Ways RPM Helps Patients With Alzheimer’s Disease
- Provides remote monitoring in the comfort of home
Remote patient monitoring systems and smartphone apps with vital sign monitoring, and wearables (e.g., activity trackers), are non-invasive and can continuously evaluate health parameters and metrics in patients with Alzheimer’s. Remote patient monitoring devices are ideal for monitoring Alzheimer’s disease patients because they may assess processes in a “real-world” situation, providing greater validity and sensitivity than in-clinic examinations.
Remote patient monitoring technologies have the potential to be more useful than traditional in-clinic examinations as they track sleep, gait, and daily activities while the patient is at home. Remote patient monitoring systems do not rely on caregiver recall, making them more objective and less stressful for people with Alzheimer’s disease.
- Ensures safety and convenience
Self-care is very important for those with Alzheimer’s disease. As a result, remote patient monitoring focuses on the patient’s specific needs. Alzheimer’s disease makes it difficult to manoeuvre properly and raises the risk of falls. Having appointments at home, without the hassle of traveling, can be safer than going to an office or clinic for monitoring.
Remote patient monitoring allows patients to effectively manage their own health while also keeping track of important information about their condition. Remote patient monitoring systems may allow Alzheimer’s patients to have 24-hour access to their care teams, treatment regimens, and personal health information. Patients who participate in remote patient monitoring may have reduced stress, improved sleep habits, and increased physical fitness.
- Reduces healthcare costs
Remote patient monitoring is also cost-effective. Remote patient monitoring allows older people to stay at home longer while still receiving the care they need. This makes the choice ideal for those who do not wish to spend their senior years in a nursing facility.
Chronically ill persons can also benefit from it, as those with Alzheimer’s disease in the later stages sometimes struggle to adjust to new surroundings. Remote patient monitoring also reduces exposure to infectious diseases in general, which can have devastating consequences for persons with Alzheimer’s disease.
With RPM, patient vital sign data is securely obtained using FDA-approved RPM devices. Cellular medical devices or Bluetooth technology allows the data to be automatically transmitted to the physician’s RPM platform and analyzed.
Furthermore, RPM allows clinicians to evaluate health and immediately adjust treatment regimens.
Wearable Devices & Sensors
RPM devices can be used to monitor a variety of health parameters, including blood pressure, heart rate, temperature, oxygen saturation, peak expiratory flow, blood glucose, and weight. Wearable gadgets, such as smart watches or activity trackers, can track vital signs including heart rate, sleep habits, and physical activity. These insights enable healthcare providers to notice irregularities or changes in patterns, which may indicate deteriorating symptoms or health hazards.
Smart home solutions that include environmental sensors can monitor Alzheimer’s patients’ everyday activities and routines. These sensors detect movements, changes in room temperature, water usage, and much more, allowing caretakers or healthcare providers to notice safety concerns and provide needed support.
Video Monitoring & Medication Management
Video monitoring systems deployed in patients’ living environments allow for remote observation and monitoring of Alzheimer’s patients and their everyday routines. These cameras protect patient safety, track sleep patterns, and evaluate cognitive and functional capabilities. When deploying video monitoring, ethical considerations and privacy must be kept in mind.
Remote patient monitoring for Alzheimer’s disease can also help with medication adherence using smart pillboxes or reminder systems. These medical gadgets notify or remind patients and caregivers when it is time to take medication. Monitoring adherence remotely allows healthcare providers to assess treatment success and intervene as needed.
Monitoring for Alzheimer’s Disease – Key Points & Takeaways
Alzheimer’s disease can significantly impair a person’s quality of life, but continuous therapy and monitoring can help prevent symptoms and enhance quality of life. The condition weakens memory, thinking, learning, and organizing skills, gradually reducing a patient’s ability to accomplish daily chores. Alzheimer’s disease is not a natural part of becoming older. However, remote patient monitoring can help people with Alzheimer’s disease by managing their chronic care.
Remote patient monitoring for Alzheimer’s disease can provide significant insights, improve patient monitoring, and boost caregiver support. While RPM should not replace regular in-person clinical visits, it improves Alzheimer’s disease monitoring and allows people to age peacefully.
Take Charge Of Alzheimer’s Remote Monitoring With HealthArc
To promote patient and caregiver engagement, a remote patient monitoring experience must be secure, accurate, and easy to use. HealthArc’s digital health platform enables healthcare providers to establish clear remote patient management goals and outcomes, making it convenient and accessible.
Our RPM software is designed to scale your healthcare results and make patient care and management easy. Our suite of FDA-approved remote monitoring devices, patient communication and interaction capabilities, a dedicated customer success team, clinical software, physician dashboard, and billing capabilities provide a comprehensive solution to ensure efficient care management for Alzheimer’s patients.
Please request a free demo to learn how we can help your organization achieve its care management goals. Also, feel free to talk to our team at +201 885 5571 for any queries.
Frequently Asked Questions (FAQs)
Remote Patient Monitoring is a program where easy-to-use home devices (e.g., blood-pressure cuff, weight scale, pulse oximeter, glucometer, thermometer, and optional wearables) send readings to the care team so they can spot concerning trends early and intervene between visits.
It supports day-to-day stability by tracking vital signs, medication routines, hydration/weight changes, sleep and activity patterns (when wearables are used), and flags deviations that may precede confusion, agitation, infections, or acute decline.
Common red flags include rising blood pressure, oxygen saturation drops, sudden weight gain or loss, fever, blood glucose excursions, missed readings suggesting routine breakdown, and unusual activity patterns (with supported wearables).
Programs aim to reduce avoidable returns by escalating sooner—coaching caregivers, adjusting care plans, or scheduling timely follow-ups when trends turn risky.
These devices typically include a cellular blood-pressure cuff, pulse oximeter, digital thermometer, weight scale, and, when applicable, a glucometer. Some programs add a simple activity wearable to help track steps, sleep regularity, and restlessness.
Not necessarily. Many kits are cellular-enabled and transmit automatically, which is advantageous for older adults or homes without broadband.
Caregivers usually help with setup and daily readings. The program should train caregivers in correct technique (proper cuff fit, posture, and measurement timing) to ensure accuracy.
Most programs follow a daily schedule for key vitals, with flexible frequency based on the individual’s conditions and risk profile. The care team may ask for extra readings when a trend is concerning.
The RPM platform flags the result according to predefined thresholds. A nurse or care coordinator reviews it, contacts the caregiver for a quick examination, and follows an escalation pathway (coaching, provider message, telehealth visit, or in-person evaluation).
Standard vitals equipment does not detect falls or locations. If these are concerns, ask about complementary options such as fall-detection pendants, bed/chair sensors, or GPS-enabled wearables.
RPM data and notes are shared with the primary and specialty teams. Programs should document changes to the care plan, notify clinicians of persistent trends, and route urgent issues per protocol.
Yes. Alzheimer’s commonly coexists with hypertension, diabetes, COPD, or heart failure. Monitoring helps manage these conditions, which in turn can reduce confusion from infections, dehydration, or medication side effects.
Thresholds are individualized based on baselines, diagnoses, and clinician guidance. Effective programs also refine thresholds over time to minimize false alarms and “alert fatigue.”
The program includes training on device use, measurement tips, red flag recognition, and what to do when alerts occur. Many teams also provide simple scripts for hydration, nutrition, sleep hygiene, and medication routines.
Consent is typically provided by the patient when possible; otherwise, by a legally authorized representative. Caregivers should be listed as contacts for alerts and coordination.
RPM programs follow medical-privacy requirements. Data transmission is encrypted, access is role-based, and audit trails are maintained. Caregivers receive only the information needed to support daily care.
Care teams verify technique, repeat the reading, and replace faulty devices when needed. Many kits include quick-swap logistics and phone support for troubleshooting.
No. RPM augments—not replaces—regular medical care. If severe symptoms appear (e.g., difficulty breathing, chest pain, sudden weakness), seek emergency care immediately.
Yes. It often pairs well with chronic care or transitional care programs to provide structured coaching, medication reviews, and follow-ups after hospital discharge.
Track simple, meaningful measures: percentage of days with successful readings, alert-to-action time, adherence to medications, stability of blood pressure and glucose, sleep regularity (if wearable used), and fewer urgent, unplanned visits.
One-button cellular devices, large displays, multilingual instructions, caregiver dashboards, reminder routines, low battery prompts, and clear escalation paths that prioritize coaching before disruption are key components of a dementia-friendly RPM program.
Create a calm measurement spot with a chair and table, keep devices together in a labeled bin, schedule readings after toileting and before breakfast when possible, and maintain a simple visual checklist for the caregiver.
Most Recent Blogs
Categories
Related Blog
- January 24, 2026 | Read Time: 15 mins
Care Gaps in Healthcare: What They Mean, and How to Close Them Faster
There has always been a lot of data in healthcare. The challenge...
Learn More- January 8, 2026 | Read Time: 11 mins
Top 5 Vitals That Drive Better Outcomes in Remote Patient Monitoring Programs
As per various studies and well documented reports on managing chronic illnesses...
Learn More- November 26, 2025 | Read Time: 14 mins
Return on Investment (ROI) of Remote Patient Monitoring (RPM): A Complete Guide for ACOs and Healthcare Organizations
The U.S. healthcare system continues its transition from fee-for-service models to value-based...
Learn More


