How CMS 2026 Medicare Proposed Rules will affect Telehealth & RPM

The CMS 2026 Medicare Physician Fee Schedule proposed rule could be the most significant telehealth and RPM shift since COVID. From removing frequency limits and expanding covered services to new RPM billing flexibility, these updates create fresh revenue opportunities but also raise compliance and operational challenges.
If you’re in healthcare, you probably felt that shift in the universe last month when CMS dropped their CY 2026 Medicare Physician Fee Schedule proposed rule. No, that wasn’t just another bureaucratic shuffle – it was the sound of telehealth barriers finally crumbling.
We’ve been diving deep into this 2,000+ page policy document (so you don’t have to), and honestly, we’re excited. This isn’t just policy wonk stuff – these changes are about to fundamentally alter how you deliver care and, frankly, how much money you can make doing it.
But here’s the thing: you’ve got until September 12, 2025 to weigh in on these changes. After that, what gets finalized is what you’re stuck with. So let’s break down what actually matters for your practice.
Table of Contents
ToggleThe Bureaucracy Finally Gets Out of Your Way
Remember that nightmare 5-step process to get telehealth services approved? The one where you needed a PhD in regulatory compliance just to figure out if your service might possibly qualify for coverage someday, maybe, if the stars aligned?
CMS basically threw that whole system in the trash.
They’re keeping the first three steps (the ones that actually make sense), but ditching the bureaucratic maze that was Steps 4 and 5. No more “provisional” versus “permanent” designations that nobody could decode. No more hunting for unicorn clinical studies to prove what you already know works.
What this actually means for you: If your service makes it onto the Medicare Telehealth Services List, it’s permanent from day one. Plan your telehealth programs with confidence instead of crossing your fingers and hoping CMS doesn’t change their mind next year.
Check how “ONE BIG BEAUTIFUL BILL” will change Telehealth.
New Services That Actually Matter
CMS approved some new telehealth services that address real gaps in virtual care:
Group Behavioural Counseling for Obesity (G0473): Finally! With over a third of American adults dealing with obesity, group counseling via telehealth eliminates the “I can’t get there” excuse. Your patients can join sessions from their living room, and you can help more people at once.
Multiple-Family Group Psychotherapy (90849): Anyone who’s tried to coordinate a family therapy session knows the logistics nightmare of getting everyone in one room at one time. Now families can join from wherever they are – whether that’s across town or across the country.
Infectious Disease Add-On (G0545): Perfect timing, right? Complex infectious diseases need frequent monitoring and consultation. Telehealth makes this possible without the “do I really need to come in?” conversations.
Auditory Services (92622 & 92623): Specialized hearing care can now reach patients who previously couldn’t access it due to transportation or mobility challenges.
The one disappointment? CMS shot down telemedicine E/M services (98000–98015). The reason? They don’t meet the separate reimbursement criteria. Sometimes bureaucracy still wins.
The Frequency Police Are Off Duty
This might be the biggest game-changer, especially if you work with hospitals or nursing facilities.
Before COVID, CMS was essentially micromanaging your clinical judgment with arbitrary limits:
- One subsequent inpatient visit every three days
- One subsequent nursing facility visit every 14 days
- One critical care consultation per day
These limitations made about as much sense as limiting how often you could check your email. Patients don’t get sick on CMS’s schedule.
Here’s what’s changing: These frequency limits are gone. Forever. For subsequent inpatient visits (99231, 99232, 99233), subsequent nursing facility visits (99307, 99308, 99309, 99310), and critical care consultations (G0508, G0509).
CMS looked at their own data and found that less than 5% of beneficiaries even received these services via telehealth, and providers rarely hit the frequency limits anyway. Their conclusion? Maybe we should trust doctors to know when their patients need care.
Translation: More billable telehealth visits. More flexibility in patient management. More revenue potential.
Virtual Supervision Becomes the New Normal
Here’s where things get operationally exciting (yes, we said operationally exciting – stick with us).
For years, “direct supervision” meant the supervising physician had to be physically in the building. COVID forced everyone to try virtual supervision through audio-video technology, and guess what? It worked just fine.
Starting January 1, 2026, virtual supervision via real-time audio-video (not just audio – you need to see what’s happening) becomes permanent for most Medicare Part B services. The exceptions are the high-risk surgical procedures (global surgery indicators 010 or 090) where in-person oversight is still required.
What this means for your operations:
- Your supervising physicians can oversee multiple locations without driving between offices
- Better staff utilization and geographic flexibility
- Reduced overhead costs for multi-site practices
- Faster response times for patient care situations
The catch: You need rock-solid audio-video technology integrated with your EHR systems. This isn’t a Zoom call – this is medical supervision that needs to meet compliance standards.
Digital Mental Health Gets Serious Investment
CMS is expanding coverage for digital mental health treatment to include FDA-authorized digital therapeutic devices for ADHD. These aren’t just apps on your phone – they’re validated medical devices that complement traditional therapy.
The technology is evolving so fast that CMS admits they don’t have enough data to set national pricing for some of these devices yet. For now, your local Medicare Administrative Contractor will determine payment rates.
But here’s the forward-looking part: CMS is actively seeking input on expanding coverage to digital therapeutics for gastrointestinal conditions, sleep disorders, and fibromyalgia. They’re not just testing the waters – they’re diving in.
Remote Monitoring Gets More Flexible
We’ll share a full breakdown in our upcoming RPM analysis, but here’s the key update: CMS is adding new billing codes that make remote patient monitoring more flexible and profitable.
What’s changing:
- Shorter management time – Providers can now bill for 10–19 minutes of monitoring and management, instead of needing to hit longer thresholds.
- Flexible data transmission – Device data no longer needs to be collected for a strict 16 days. The new rules allow 2–15 day reporting periods to qualify.
For organizations already using advanced RPM platforms, these changes create immediate new revenue opportunities while making it easier to engage more patients.
Check our complete guide to Remote Patient Monitoring – HERE
Financial Updates: Small but Meaningful
The telehealth originating site facility fee is increasing from $31.01 to $31.85 for 2026. Not exactly retirement money, but it shows CMS’s commitment to maintaining the financial viability of telehealth infrastructure.
The real money is in the expanded services, eliminated frequency limits, and new remote monitoring codes. We’re talking about fundamental changes to revenue streams, not just cost-of-living adjustments.
To know more about Pricing Structure and models of RPM –READ MORE
What’s Still Missing and Why It Matters
One issue CMS left unresolved—despite strong provider support—was whether practitioners can list their practice location instead of their home address when delivering telehealth visits.
It may sound like a small paperwork detail, but it has major implications for safety, privacy, and operational efficiency. Many providers raised concerns about having their personal home addresses appear in billing systems and pushed hard for this flexibility, but CMS has not yet made the change.
It’s worrying that no one is talking about this, especially since this flexibility was extended to 2025 with significant support from stakeholders. If this matters to your practice, the comment period is your chance to make your voice heard.
The September 30th Cliff Nobody’s Talking About
Here’s the uncomfortable truth: While CMS is expanding telehealth services, the underlying COVID-19 flexibilities that make telehealth accessible are set to expire on September 30, 2025.
These include:
- Waived geographic restrictions (rural-only requirements)
- Allowing patients’ homes as originating sites
- Cross-state licensing flexibilities
Without Congressional action, we could end up with expanded telehealth services that fewer patients can actually access. It’s like building a beautiful highway that doesn’t connect to any roads.
What You Should Do Right Now
Before September 12, 2025:
- Read the proposed rule (or at least the sections relevant to your practice)
- Submit comments if these changes affect your operations
- Start assessing your technology infrastructure – especially for virtual supervision requirements
Before January 1, 2026:
- Upgrade your audio-video capabilities if you plan to use virtual supervision
- Train your staff on new billing codes and documentation requirements
- Update your policies and procedures to reflect new flexibilities
- Model the financial impact of frequency limit removal and new services
Throughout 2026:
- Monitor your results – track revenue, efficiency, and patient outcomes
- Optimize your processes based on real-world experience
- Stay engaged with ongoing policy developments
Why This Matters for Digital Health
At HealthArc, we’ve been watching the slow evolution of telehealth policy for years. These changes represent the biggest leap forward since the COVID emergency declarations.
It is not merely the specific policy changes that are important to us but what they imply: CMS is now recognizing and accepting telehealth as a legitimate method of healthcare delivery, instead of an emergency stop-gap measure. They are taking the clinical judgment of providers rather than trying to hold on micro-control of all interactions.
To organizations with established digital health tools, infrastructure, and platforms, the shifts are competitive benefits in their own right. You are correspondingly ready to take advantage of the available opportunities.
To the rest of the players doing so yet, this is your wake up call. The telehealth train is no longer coming, it is here, it is gaining speed and you need to hop on.
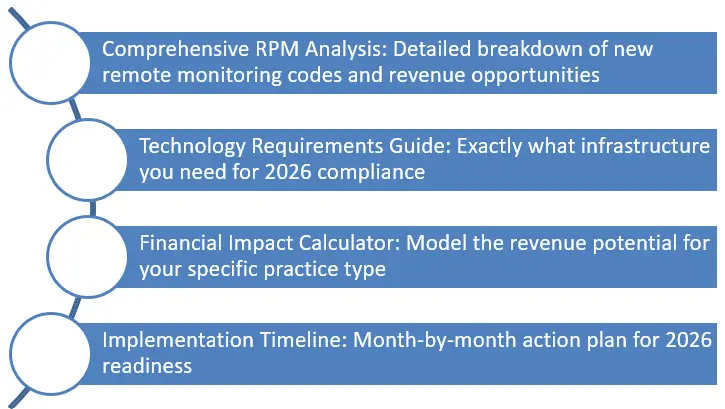
Coming Up: Deep Dive Analysis
This overview provides you with the strategic landscape, but the implementation details are crucial. Over the next few weeks, we’ll be publishing:
The Bottom Line
Medicare just handed healthcare providers the most significant expansion of virtual care opportunities in the program’s history. The question isn’t whether these changes will impact your practice – it’s whether you’ll be ready to maximize their potential.
CMS has made it clear: the future of healthcare includes virtual care as a permanent, integral component. They’re removing barriers, expanding coverage, and trusting providers to use their professional judgment.
Now it’s your turn to decide how to use these tools to deliver better care and build a more sustainable practice.
Want personalized analysis of how these changes impact your organization? Our team at HealthArc specializes in helping healthcare providers navigate policy changes and implement technology solutions that drive results. Let’s talk about preparing your practice for the opportunities ahead.
Key Takeaways
- CMS 2026 brings the biggest telehealth & RPM update since COVID.
- Barriers removed: frequency limits, complex approvals.
- New codes expand RPM flexibility and reimbursement.
- Providers gain more opportunities but face compliance challenges.
- HealthArc helps practices adapt quickly with scalable, audit-ready solutions.
Frequently Asked Questions (FAQs)
It’s a policy update released July 2025 that reshapes telehealth and RPM reimbursement.
Most provisions take effect January 1, 2026.
- Simplified approval process
- Permanent coverage for approved services
- Removal of visit frequency limits
Group behavioral counseling, multi-family psychotherapy, infectious disease add-on, and auditory services.
Old restrictions on inpatient, nursing facility, and critical care telehealth visits are permanently removed.
Physicians can oversee staff remotely via real-time video for most services, reducing overhead and improving flexibility.
New codes allow shorter data collection periods (2–15 days) and 10–19 min management billing.
Expanded codes and service coverage create more billable opportunities and improved reimbursement flexibility.
- Documentation and compliance demands
- Training staff on new codes
- Infrastructure needs for virtual supervision
On Sept 30, 2025, pandemic-era flexibilities (home sites, cross-state care) may expire without Congressional action.
Primary care, specialty practices (cardiology, endocrinology), post-surgical care teams, and large health systems.
- Upgrade telehealth & RPM platforms
- Train staff on new codes and documentation
- Engage in advocacy for waiver extensions
- Model financial impact of new reimbursement structures
HealthArc’s RPM and telehealth platform integrates devices, AI dashboards, compliance automation, and billing tools to simplify 2026 transitions.
The CMS 2026 changes will reshape how providers earn from Remote Patient Monitoring, creating both new revenue opportunities and compliance considerations. Read the full breakdown here: Impact of CMS 2026 Changes on RPM Revenue
Most Recent Blogs
Categories
Related Blog
- February 27, 2026 | Read Time: 11 mins
What Is the CMS Access Model? A Complete Guide for Healthcare Providers
The CMS Access Model represents a significant shift in how Medicare reimburses...
Learn More- February 13, 2026 | Read Time: 8 mins
CPT 99445 and 99470: Complete 2026 Guide to Short-Window RPM Billing with HealthArc
CPT 99445 and CPT 99470 are transforming how practices bill for Remote...
Learn More- January 20, 2026 | Read Time: 13 mins
The Future of Care is at Home, Driven by the Rapid Expansion of Hospital-At-Home Programs.
Healthcare is evolving. A model that brings hospital-level services directly into patients'...
Learn More


